REVIEW PAPER
Environmental factors of melanoma and use of artificial intelligence in its diagnosis – narrative review
1
Center for Digital Transformation and Prototype Solutions., Lukasiewicz Research Network - Lodz Institute of Technology
2
Research Department, Uczelnia Medyczna im. Marii Skłodowskiej-Curie, Warszawa, Polska
3
Research and development, Maria Sklodowska-Curie Diagnostic Center Ltd.
4
Badania i rozwój, Centrum Diagnostyczne im. Marii Skłodowskiej-Curie, Warszawa, Polska
These authors had equal contribution to this work
Corresponding author
Sebastian Górecki
Centrum Cyfrowej Transformacji i Rozwiązań Prototypowych, Sieć Badawcza Łukasiewicz – Łódzki Instytut Technologiczny
Centrum Cyfrowej Transformacji i Rozwiązań Prototypowych, Sieć Badawcza Łukasiewicz – Łódzki Instytut Technologiczny
Med Srod. 2025;28(2):52-59
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
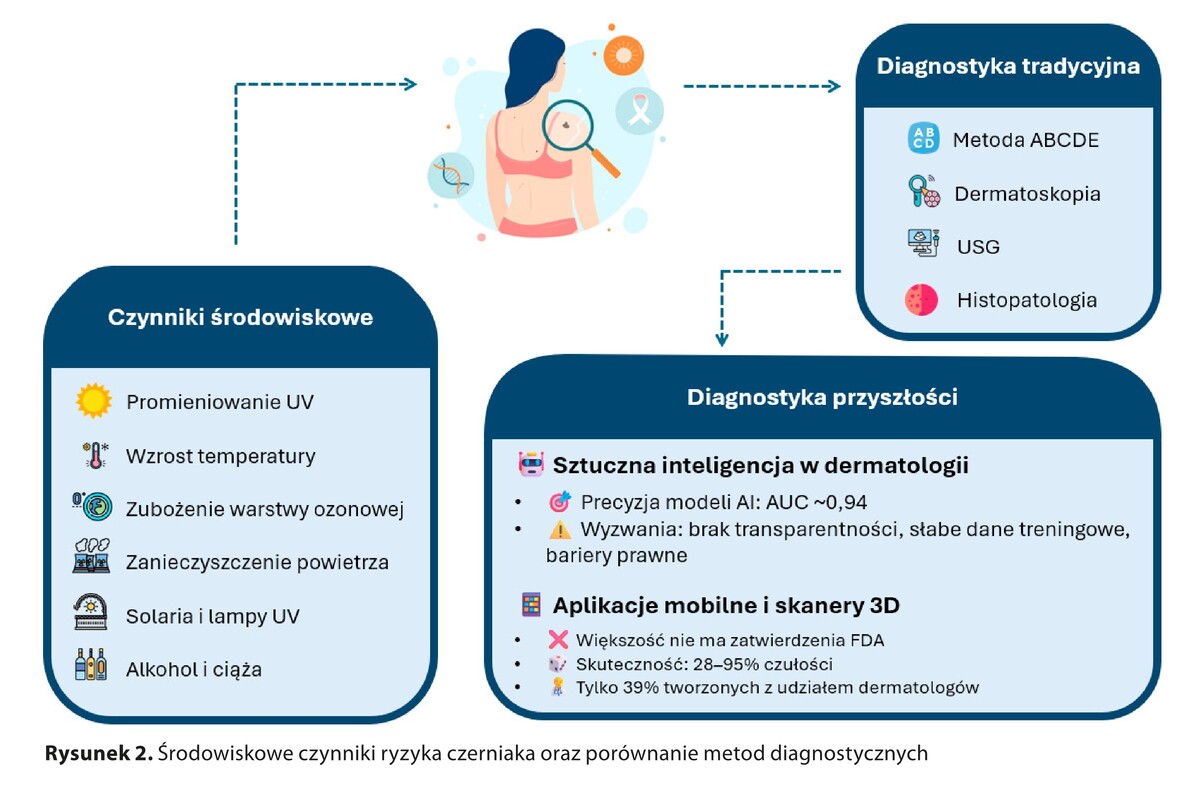
Melanoma is a highly aggressive skin cancer with a rising incidence worldwide. Its development is influenced by a combination of genetic predisposition and environmental factors, such as UV radiation, pollution, and exposure to harmful chemicals. The prognosis of melanoma is strongly linked to early diagnosis, as survival rates drop significantly in advanced stages. This study aims to examine how environmental factors contribute to the risk of melanoma and explore the potential of artificial intelligence (AI) in supporting its early detection.
Abbreviated description of the state of knowledge:
Conventional diagnostic approaches, including dermoscopy and histopathology, remain the gold standard of melanoma detection. However, their effectiveness depends on clinician expertise and access to specialized equipment, which can be limiting. In recent years, AI-driven methods, particularly convolutional neural networks (CNNs), have gained prominence for their ability to analyze medical images with high accuracy. AI-based tools can assist in the classification of skin lesions, facilitating earlier and more precise diagnosis, which is crucial for improving treatment outcomes.
Summary:
The integration of AI with classic diagnostic methods has the potential to enhance accuracy, streamline clinical processes, and reduce misdiagnosis rates. Nevertheless, further validation studies and regulatory approvals are essential before AI systems can be widely implemented in clinical practice. Beyond technological advancements, raising public awareness of melanoma risk factors and promoting preventive strategies remain vital in reducing the incidence of this disease.
Melanoma is a highly aggressive skin cancer with a rising incidence worldwide. Its development is influenced by a combination of genetic predisposition and environmental factors, such as UV radiation, pollution, and exposure to harmful chemicals. The prognosis of melanoma is strongly linked to early diagnosis, as survival rates drop significantly in advanced stages. This study aims to examine how environmental factors contribute to the risk of melanoma and explore the potential of artificial intelligence (AI) in supporting its early detection.
Abbreviated description of the state of knowledge:
Conventional diagnostic approaches, including dermoscopy and histopathology, remain the gold standard of melanoma detection. However, their effectiveness depends on clinician expertise and access to specialized equipment, which can be limiting. In recent years, AI-driven methods, particularly convolutional neural networks (CNNs), have gained prominence for their ability to analyze medical images with high accuracy. AI-based tools can assist in the classification of skin lesions, facilitating earlier and more precise diagnosis, which is crucial for improving treatment outcomes.
Summary:
The integration of AI with classic diagnostic methods has the potential to enhance accuracy, streamline clinical processes, and reduce misdiagnosis rates. Nevertheless, further validation studies and regulatory approvals are essential before AI systems can be widely implemented in clinical practice. Beyond technological advancements, raising public awareness of melanoma risk factors and promoting preventive strategies remain vital in reducing the incidence of this disease.
REFERENCES (50)
1.
Miller KD, Fidler-Benaoudia M, Keegan TH, et al. Cancer statistics for adolescents and young adults, 2020. CA Cancer J Clin. 2020;70:443–459. https://doi.org/10.3322/caac.2....
2.
Ostrowski SM, Fisher DE. Biology of melanoma. Hematol/Oncol Clin North Am. 2021;35:29–56. https://doi.org/10.1016/j.hoc.....
3.
Loras A, Gil-Barrachina M, Marqués-Torrejón MÁ, et al. UV-induced somatic mutations driving clonal evolution in healthy skin, nevus, and cutaneous melanoma. Life 2022;12:1339. https://doi.org/10.3390/life12....
4.
McMeniman EK, Duffy DL, Jagirdar K, et al. The interplay of sun damage and genetic risk in Australian multiple and single primary melanoma cases and controls. Br J Dermatol. 2020;183:357–366. https://doi.org/10.1111/bjd.18....
5.
Berman-Rosa M, Logan J, Ghazawi FM, et al. Analysis of geographic and environmental factors and their association with cutaneous melanoma incidence in Canada. Dermatol. 2022;238:1006–1017. https://doi.org/10.1159/000524....
6.
Watson TPG, Tong M, Bailie J, et al. Relationship between climate change and skin cancer and implications for prevention and management: A scoping review. Public Health. 2024;227:243–249. https://doi.org/10.1016/j.puhe....
7.
Lagacé F, Noorah BN, Conte S, et al. Assessing skin cancer risk factors, sun safety behaviors and melanoma concern in Atlantic Canada: A comprehensive survey study. Cancers (Basel). 2023;15:0000. https://doi.org/10.3390/cancer....
8.
McDonald KA, Lytvyn Y, Mufti A, et al. Review on photoprotection: A clinician’s guide to the ingredients, characteristics, adverse effects, and disease-specific benefits of chemical and physical sunscreen compounds. Arch Dermatol Res. 2022;315:735–749. https://doi.org/10.1007/s00403....
9.
Lapides R, Saravi B, Mueller A, et al. Possible explanations for rising melanoma rates despite increased sunscreen use over the past several decades. Cancers (Basel). 2023;15:5868. https://doi.org/10.3390/cancer....
10.
Alli S, LeBeau J, Hasbani A, et al. Understanding the perceived relationship between sun exposure and melanoma in Atlantic Canada: A consensual qualitative study highlighting a „sunscreen paradox.” Cancers (Basel). 2023;15:4726. https://doi.org/10.3390/cancer....
11.
An S, Kim K, Moon S, et al. Indoor tanning and the risk of overall and early-onset melanoma and non-melanoma skin cancer: Systematic review and meta-analysis. Cancers 2021;13:5940. https://doi.org/10.3390/cancer....
12.
Burgard B, Reichrath J. Solarium use and risk for malignant melanoma: Many open questions, not the time to close the debate. Sunlight Vitam D Skin Cancer. 2020;155–170. https://doi.org/10.1007/978-3-....
13.
Rastrelli M, Tropea S, Rossi CR, Alaibac M. Melanoma: epidemiology, risk factors, pathogenesis, diagnosis and classification. In Vivo. 2014;28(6):1005–11.
14.
López Figueroa F. Implicaciones dermatológicas del cambio climático y de la disminución de la capa de ozono. Actas Dermosifiliogr. 2011;102:311–315. https://doi.org/10.1016/j.ad.2....
15.
Van Dijk A, Slaper H, den Outer PN, et al. Skin cancer risks avoided by the Montreal Protocol-worldwide modeling integrating coupled climate-chemistry models with a risk model for UV. Photochem Photobiol. 2012;89:234–246. https://doi.org/10.1111/j.1751....
16.
Lee H, Kim OJ, Jung J, et al. Long-term exposure to particulate air pollution and incidence of Parkinson’s disease: A nationwide population-based cohort study in South Korea. Environ Res. 2022;212:113165. https://doi.org/10.1016/j.envr....
17.
Liu J, Chen Y, Cao H, Zhang A. Burden of typical diseases attributed to the sources of PM2.5-bound toxic metals in Beijing: An integrated approach to source apportionment and QALYs. Environ Int. 2019;131:105041. https://doi.org/10.1016/j.envi....
18.
Burke KE. Mechanisms of aging and development – a new understanding of environmental damage to the skin and prevention with topical antioxidants. Mech Ageing Dev. 2018;172:123–130. https://doi.org/10.1016/j.mad.....
19.
Schraufnagel DE, Balmes JR, Cowl CT, et al. Air pollution and noncommunicable diseases. Chest 2019;155:409–16. https://doi.org/10.1016/j.ches....
20.
Behrens G, Niedermaier T, Berneburg M, et al. Physical activity, cardiorespiratory fitness and risk of cutaneous malignant melanoma: Systematic review and meta-analysis. PLOS ONE 2018;13:e0206087. https://doi.org/10.1371/journa....
21.
Yamauchi T, Shangraw S, Zhai Z, et al. Alcohol as a non-UV social-environmental risk factor for melanoma. Cancers. 2022;14:5010. https://doi.org/10.3390/cancer....
22.
Rota M, Pasquali E, Bellocco R, et al. Alcohol drinking and cutaneous melanoma risk: A systematic review and dose-risk meta-analysis. Br J Dermatol. 2014;170:1021–1028. https://doi.org/10.1111/bjd.12....
23.
Kubo JT, Henderson MT, Desai M, et al. Alcohol consumption and risk of melanoma and non-melanoma skin cancer in the Women’s Health Initiative. Cancer Causes Control. 2013;25:1–10. https://doi.org/10.1007/s10552....
24.
Born LJ, Tembunde Y, Driscoll MS, Grant-Kels JM. Melanoma and melanocytic nevi in pregnancy. Clin Dermatol. 2025. https://doi.org/10.1016/j.clin....
25.
Lee Y, Roberts C, Dobbins T, et al. Incidence and outcomes of pregnancy-associated cancer in Australia, 1994–2008: A population-based linkage study. BJOG. 2012;119:1572–1582. https://doi.org/10.1111/j.1471....
26.
Zelin E, Conforti C, Giuffrida R, et al. Melanoma in pregnancy: Certainties unborn. Melanoma Management 2020;7. https://doi.org/10.2217/mmt-20....
27.
Głuszek J, Kosicka TM. Wpływ smogu (zanieczyszczonego powietrza) na choroby układu sercowo-naczyniowego. Choroby Serca i Naczyń 2019;16:201–6. https://doi.org/10.5603/chsin.....
28.
Carter TJ, George C, Harwood C, Nathan P. Melanoma in pregnancy: Diagnosis and management in early-stage and advanced disease. Eur J Cancer. 2022;166:240–253. https://doi.org/10.1016/j.ejca....
29.
Metko D, Mehta S, McMullen E, et al. A systematic review of the risk of cutaneous malignancy associated with ultraviolet nail lamps: What is the price of beauty? Eur J Dermatol. 2024;34:26–30. https://doi.org/10.1684/ejd.20....
30.
UK CR. Melanoma skin cancer survival statistics — cancerresearchuk.org;. [Accessed 16-02-2025]. https://www.cancerresearchuk.o....
31.
Chatzilakou E, Hu Y, Jiang N, et al. Biosensors for melanoma skin cancer diagnostics. Biosens Bioelectron. 2024;250:116045. https://doi.org/10.1016/j.bios....
32.
Kasmi R, Mokrani K. Classification of malignant melanoma and benign skin lesions: Implementation of automatic ABCD rule. IET Image Process. 2016;10:448–455. https://doi.org/10.1049/iet-ip....
33.
Williams NM, Rojas KD, Reynolds JM, et al. Assessment of diagnostic accuracy of dermoscopic structures and patterns used in melanoma detection: A systematic review and meta-analysis. JAMA Dermatol. 2021;157:1078. https://doi.org/10.1001/jamade....
34.
Pathania YS, Apalla Z, Salerni G, et al. Non-invasive diagnostic techniques in pigmentary skin disorders and skin cancer. J Cosmet Dermatol. 2021;21:444–450. https://doi.org/10.1111/jocd.1....
35.
Wortsman X. Ultrasound in skin cancer: Why, how, and when to use it? Cancers 2024;16:3301. https://doi.org/10.3390/cancer....
36.
Asato MA, Moares-Neto FA, Toledo Moraes MP de, et al. Depth of invasion analysis to predict acral melanoma outcomes. Ann Diagnostic Pathol 2024;71:152305. https://doi.org/10.1016/j.annd....
37.
Bissoto A, Perez F, Valle E, et al. Skin lesion synthesis with generative adversarial networks 2019. https://doi.org/10.48550/ARXIV....
38.
Tschandl P. The HAM10000 dataset, a large collection of multi-source dermatoscopic images of common pigmented skin lesions 2018. https://doi.org/10.7910/DVN/DB....
39.
Kreouzi M, Theodorakis N, Feretzakis G, et al. Deep learning for melanoma detection: A deep learning approach to differentiating malignant melanoma from benign melanocytic nevi. Cancers 2024;17:28. https://doi.org/10.3390/cancer....
40.
Thomas L, Hyde C, Mullarkey D, et al. Real-world post-deployment performance of a novel machine learning-based digital health technology for skin lesion assessment and suggestions for post-market surveillance. Front Med. 2023;10. https://doi.org/10.3389/fmed.2....
41.
Bhojane S, Shrestha K, Bharadwaj S, et al. Automated skin cancer detection web-based application and review of some image classification algorithm. SSRN Elect J. 2020. https://doi.org/10.2139/ssrn.3....
42.
Strzelecki M, Kociołek M, Strąkowska M, et al. Artificial intelligence in the detection of skin cancer: State of the art. Clin Dermatol. 2024;42:280–295. https://doi.org/10.1016/j.clin....
43.
Brancaccio G, Balato A, Malvehy J, et al. Artificial intelligence in skin cancer diagnosis: A reality check. J Invest Dermatol. 2024;144:492–9. https://doi.org/10.1016/j.jid.....
44.
Wongvibulsin S, Yan MJ, Pahalyants V, et al. Current state of dermatology mobile applications with artificial intelligence features. JAMA Dermatol. 2024;160:646–50. https://doi.org/10.1001/jamade....
45.
Heinlein L, Maron RC, Hekler A, et al. Prospective multicenter study using artificial intelligence to improve dermoscopic melanoma diagnosis in patient care. Commun Med. 2024;4. https://doi.org/10.1038/s43856....
46.
Papachristou P, Söderholm M, Pallon J, et al. Evaluation of an artificial intelligence-based decision support for the detection of cutaneous melanoma in primary care: A prospective real-life clinical trial. Br J Dermatol. 2024;191:125–133. https://doi.org/10.1093/bjd/lj....
47.
Sun MD, Kentley J, Mehta P, et al. Accuracy of commercially available smartphone applications for the detection of melanoma. British J Dermatol. 2022;186:744–6. https://doi.org/10.1111/bjd.20....
48.
Jones OT, Matin RN, Schaar M van der, et al. Artificial intelligence and machine learning algorithms for early detection of skin cancer in community and primary care settings: A systematic review. The Lancet Digital Health 2022;4:e466–76. https://doi.org/10.1016/S2589-....
49.
Mar VJ, Soyer HP. Artificial intelligence for melanoma diagnosis: How can we deliver on the promise? Ann Oncol. 2019;30:e1–3. https://doi.org/10.1093/annonc....
50.
Ahmedt-Aristizabal D, Nguyen C, Tychsen-Smith L, et al. Monitoring of pigmented skin lesions using 3D whole body imaging. Comp Methods Progr Biomed. 2023;232:107451. https://doi.org/10.1016/j.cmpb....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.