RESEARCH PAPER
Environmental factors and severity of disability in selected spinal disorders-pilot study
1
Instytut Zdrowia Publicznego, Zakład Zdrowia i Środowiska, Uniwersytet Jagielloński – Collegium Medicum, Wydział Nauk o Zdrowiu, Polska
Corresponding author
Monika Ścibor
Instytut Zdrowia Publicznego/Zakład Zdrowia i Środowiska, Uniwersytet Jagielloński Collegium Medicum Wydział Nauk o Zdrowiu, Skawińska 8, 31-066, Kraków, Polska
Instytut Zdrowia Publicznego/Zakład Zdrowia i Środowiska, Uniwersytet Jagielloński Collegium Medicum Wydział Nauk o Zdrowiu, Skawińska 8, 31-066, Kraków, Polska
Med Srod. 2025;28(1):11-17
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
According to recent epidemiological data, approximately 70% of the population experience lumbosacral pain, and 50% cervical spine pain before reaching the age of 40. These conditions represent a serious medical, social and economic problem. Many environmental factors exert an effect on the development of spinal disorders: lack of physical activity, poor work ergonomics, spinal overload, advanced age, overweight and behavioural factors. Objective: The aim of the study was to assess the severity of disability caused by spinal pain, with consideration of the impact of environmental factors.
Material and methods:
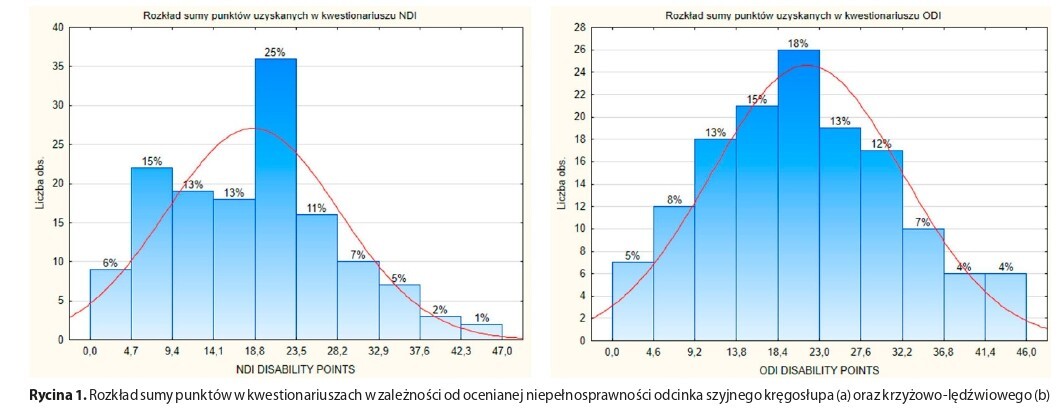
The study group consisted of 142 people suffering from spinal disorders. Their level of disability was assessed using an anonymous questionnaire based on the Neck Disability Index (NDI) and the Oswestry Disability Index (ODI). Additionally, demographic data were collected, such as age, gender, body mass index (BMI), type of occupation performed, place of residence, and the level of physical activity.
Results:
The study demonstrated that age, the lack or insufficient physical activity (once-twice per week), and place of residence are factors significantly affecting the severity of disability. However, no such relationship was found between body mass index (BMI), type of occupation, or gender. The evaluation of the relationship between different types of spinal disorders and the severity of disability revealed that the type of disorders significantly affects the level of disability
Conclusions:
There is a need to clarify and expand healthcare programmes, particularly in the areas where medical services are observed to be deficient. Educational support for the population is recommended, which may contribute to the reduction of the prevalence of spinal pain resulting especially from lack of adequate physical activity.
According to recent epidemiological data, approximately 70% of the population experience lumbosacral pain, and 50% cervical spine pain before reaching the age of 40. These conditions represent a serious medical, social and economic problem. Many environmental factors exert an effect on the development of spinal disorders: lack of physical activity, poor work ergonomics, spinal overload, advanced age, overweight and behavioural factors. Objective: The aim of the study was to assess the severity of disability caused by spinal pain, with consideration of the impact of environmental factors.
Material and methods:
The study group consisted of 142 people suffering from spinal disorders. Their level of disability was assessed using an anonymous questionnaire based on the Neck Disability Index (NDI) and the Oswestry Disability Index (ODI). Additionally, demographic data were collected, such as age, gender, body mass index (BMI), type of occupation performed, place of residence, and the level of physical activity.
Results:
The study demonstrated that age, the lack or insufficient physical activity (once-twice per week), and place of residence are factors significantly affecting the severity of disability. However, no such relationship was found between body mass index (BMI), type of occupation, or gender. The evaluation of the relationship between different types of spinal disorders and the severity of disability revealed that the type of disorders significantly affects the level of disability
Conclusions:
There is a need to clarify and expand healthcare programmes, particularly in the areas where medical services are observed to be deficient. Educational support for the population is recommended, which may contribute to the reduction of the prevalence of spinal pain resulting especially from lack of adequate physical activity.
REFERENCES (19)
1.
Friedly J, Standaert C, Chan L. Epidemiology of spine care: the back pain dilemma. Phys Med Rehabil Clin N Am. 2010;21(4):659. https://doi.org/10.1016/j.pmr.....
2.
Gibbs D, McGahan BG, Ropper AE, et al. Back pain: Differential diagnosis and management. Neurol Clin. 2023;41(1):61–76. https://doi.org/10.1016/j.ncl.....
3.
Marcinkowski J, Konopielko Z. Tajemnicze bóle kręgosłupa odcinka lędźwiowo-krzyżowego. W kręgach wiedzy, wątpliwości i kontrowersji: epidemiologów, lekarzy, fizjoterapeutów i psychologów. Zielona Góra: Uniwersytet Zielonogórski; 2023. p. 304.
4.
Vernon H, Mior S. The neck disability index: A study of reliability and validity. J Manipulative Physiol Ther. 1991;14(7):409–415.
5.
Fairbank JC, Couper J, Davies JB, O'Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980; 66(8): 271–273.
6.
Fjeld OR, Grøvle L, Helgeland J, et al. Complications, reoperations, readmissions, and length of hospital stay in 34,639 surgical cases of lumbar disc herniation. Bone Joint J. 2019;101(4):470–477. https://doi.org/10.1302/0301-6....
7.
Koszela K. Dyskopatia – czy zawsze przyczyną dolegliwości bólowych kręgosłupa? https://podyplomie.pl/medycyna... (access: 2025.02.14).
8.
Diebo BG, Shah NV, Boachie-Adjei O, et al. Adult spinal deformity. Lancet. 2019 Jul 13;394(10193):160–172. https://doi.org/10.1016/S0140-....
9.
Kruszewski A, Krajewska-Kułak E, Śmigielska-Kuzia J. Główne dolegliwości wieku podeszłego ze szczególnym uwzględnieniem schorzeń kręgosłupa. In: Krajewska-Kułak E, Łukaszuk C, Lewko J, Kułak W, editor. Holistyczny wymiar współczesnej medycyny. T. 5: praca zbiorowa. Lublin: Wydawnictwo Naukowe NeuroCentrum; 2019. p. 14–27.
10.
Wettstein M, Eich W, Bieber C, Tesarz J. Pain intensity, disability, and quality of life in patients with chronic low back pain: Does age matter? Pain Med. 2019; 20(3): 464–475. https://doi.org/10.1093/pm/pny....
11.
Leite HR, Dario AB, Harmer AR, et al. Contributions of birthweight, annualised weight gain and BMI to back pain in adults: A population-based co-twin control study of 2754 Australian twins. Eur Spine J. 2019;28(2):224–233.
12.
Lechowski Ł, Jasion A. Spatial accessibility of primary health care in rural areas in Poland. Int J Environ Res Public Health. 2021;18(17):9282. https://doi.org/10.3390/ijerph....
13.
Wojciechowski Ł. Wpływ aktywności fizycznej pracy stojącej i siedzącej na stan funkcjonalny kręgosłupa. https://www.rehabilitacja.pl (access: 10.04.2024).
14.
Leivas EG, Corrêa LA, Nogueira LAC. The relationship between low back pain and the basic lumbar posture at work: a retrospective cross-sectional study. Int Arch Occup Environ Health. 2022;1–9.
15.
Roren A, Daste C, Coleman M, et al. Physical activity and low back pain: A critical narrative review. Ann Phys Rehabil Med. 2023;66(2):101650. https://doi.org/10.1016/j.reha....
16.
Celej-Szuster J, Turowski K, Zdanowicz T, et al. Wpływ bólu na funkcjonowanie chorych z dyskopatią lędźwiową. In: Turowski K, editor. Medyczne wymiary dobrostanu. Lublin: Wydawnictwo Naukowe NeuroCentrum; 2018. p. 55–66.
17.
Malec-Milewska M. Ból zapalny w narządzie ruchu. Medycyna Faktów. 2022;15(2):216–221. https://doi.org/10.24292/01.MF....
18.
Maślińska M, Olesińska M. W gabinecie lekarza specjalisty. Choroby reumatyczne. Ból w chorobach reumatycznych. Warszawa: PZWL Wydawnictwo Lekarskie; 2022. p. 89–95, 101–114.
19.
Wettstein M, Eich W, Bieber C, Tesarz J. Pain intensity, disability, and quality of life in patients with chronic low back pain: Does age matter? Pain Med. 2019; 20(3): 464–476. https://doi.org/10.1093/pm/pny....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.