REVIEW PAPER
Infections of Cryptosporidium spp. in the context of climate change and urbanization
1
Faculty of Medicine, Medical University, Wrocław, Poland
2
Department of Population Health, Department of Public Health, Medical University, Wrocław, Poland
Corresponding author
Karolina Pawłuszkiewicz
Wydział Lekarski, Uniwersytet Medyczny im. Piastów Śląskich we Wrocławiu, wyb. Ludwika Pasteura 1, 50-367, Wrocław, Polska
Wydział Lekarski, Uniwersytet Medyczny im. Piastów Śląskich we Wrocławiu, wyb. Ludwika Pasteura 1, 50-367, Wrocław, Polska
Med Srod. 2025;28(1):6-10
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
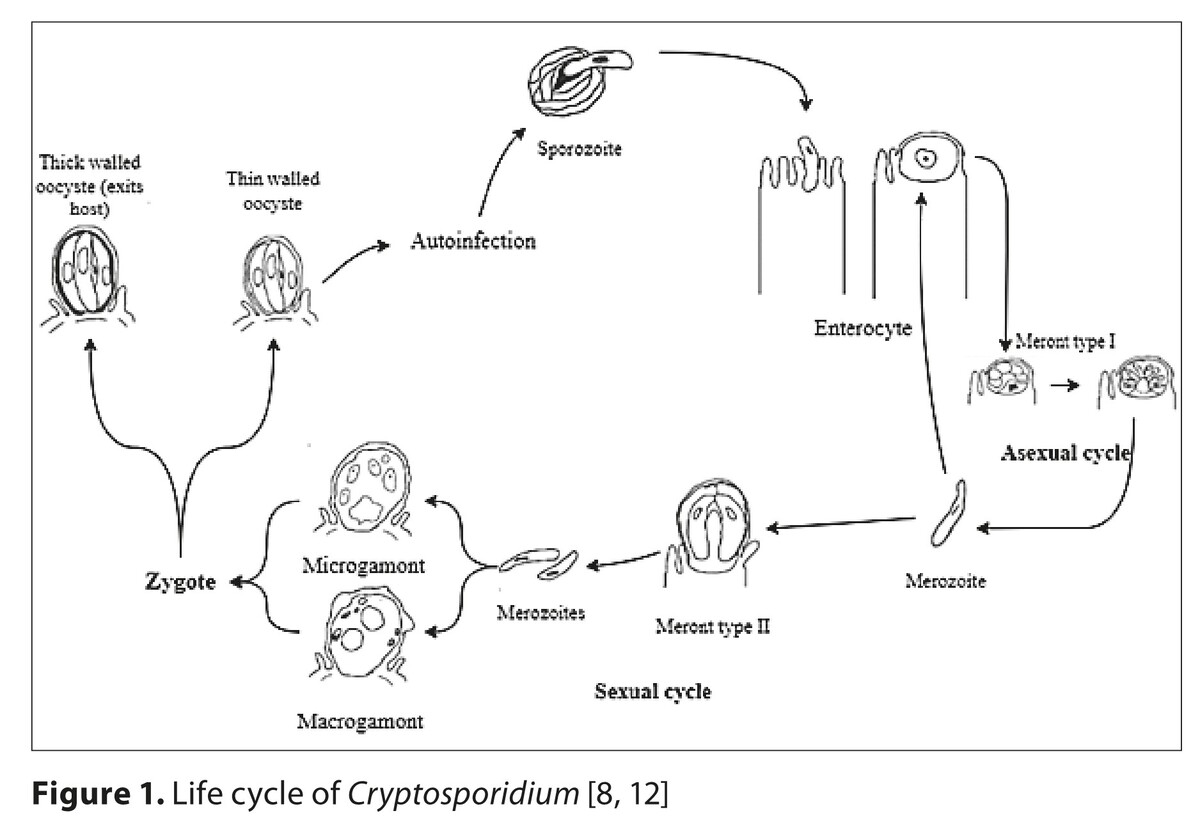
Cryptosporidium spp. are protozoans which are responsible for one of the most common waterborne disease, cryptosporidiosis. This disease is dangerous for children, immunocompromised individuals, and the residents of regions with limited access to sanitation infrastructure. Current climate change and urbanization significantly affect the transmission of these pathogens, increasing the risk of infection and causing challenges for public health. Our study analyzes the impact of urbanization and current climate changes on cryptosporidium epidemiology, with special focus on health consequences and current wastewater treatment methods.
Brief description of the state of knowledge:
Heavy rainfall, rising temperatures and extreme weather events, such as floods, promote the survival of Cryptosporidium spp. oocysts, which may spread in the surface waters. The risk of transmission is significantly exacerbated in areas with a high population density and inadequate sanitation infrastructure, leading to heightened exposure and vulnerability. Oocysts, which are highly resistant to traditional disinfection methods, such as chlorination, are able to complicate prevention efforts. Current wastewater treatment methods are physical methods – filtration and sedimentation, biological processes – activated sludge and biofiltration, and chemical methods – disinfection of contaminated water.
Summary:
Climate change and urbanization significantly increase the risk of Cryptosporidium spp. infections. Developing more effective wastewater treatment, new therapies and vaccines remain priorities, especially for protecting high-risk groups, such as young children, the elderly, and immunocompromised individuals.
Cryptosporidium spp. are protozoans which are responsible for one of the most common waterborne disease, cryptosporidiosis. This disease is dangerous for children, immunocompromised individuals, and the residents of regions with limited access to sanitation infrastructure. Current climate change and urbanization significantly affect the transmission of these pathogens, increasing the risk of infection and causing challenges for public health. Our study analyzes the impact of urbanization and current climate changes on cryptosporidium epidemiology, with special focus on health consequences and current wastewater treatment methods.
Brief description of the state of knowledge:
Heavy rainfall, rising temperatures and extreme weather events, such as floods, promote the survival of Cryptosporidium spp. oocysts, which may spread in the surface waters. The risk of transmission is significantly exacerbated in areas with a high population density and inadequate sanitation infrastructure, leading to heightened exposure and vulnerability. Oocysts, which are highly resistant to traditional disinfection methods, such as chlorination, are able to complicate prevention efforts. Current wastewater treatment methods are physical methods – filtration and sedimentation, biological processes – activated sludge and biofiltration, and chemical methods – disinfection of contaminated water.
Summary:
Climate change and urbanization significantly increase the risk of Cryptosporidium spp. infections. Developing more effective wastewater treatment, new therapies and vaccines remain priorities, especially for protecting high-risk groups, such as young children, the elderly, and immunocompromised individuals.
REFERENCES (37)
1.
Sokic-Milutinovic A, Pavlovic-Markovic A, Tomasevic RS, et al. Diarrhea as a Clinical Challenge: General Practitioner Approach. Dig Dis. 2022;40(3):282–289. doi:10.1159/000517111.
2.
Worku T, Haile T, Sahile S, et al. Parasitic etiology of diarrhea and associated factors among under-five-year children attending Mizan-Tepi University Teaching Hospital, Southwest Ethiopia. Pan Afr Med J. 2023;45:187. Published 2023 Aug 30. doi:10.11604/pamj.2023.45.187.38263.
3.
Firas A, Ibrahim A, Marwa J, et al. Cryptosporidium infection in humans and animals from Iraq: A review. Acta Trop. 2021;220:105946. doi:10.1016/j.actatropica.2021.105946.
4.
Wang X, Wang X, Cao J. Environmental Factors Associated with Cryptosporidium and Giardia. Pathogens. 2023;12(3):420. doi:10.3390/pathogens12030420.
5.
Ikiroma IA, Pollock KG. Influence of weather and climate on crypto -sporidiosis-A review. Zoonoses Public Health. 2021;68(4):285–298. doi:10.1111/zph.12785.
6.
Poglayen G, Gelati A, Scala A, et al. Do natural catastrophic events and exceptional climatic conditions also affect parasites? Parasitology. 2023;150(12):1158–1166. doi:10.1017/S0031182023000471.
7.
Nasser AM. Removal of Cryptosporidium by wastewater treatment processes: a review. J Water Health. 2016;14(1):1–13. doi:10.2166/wh.2015.131.
8.
Thompson RC, Olson ME, Zhu G, et al. Cryptosporidium and cryptosporidiosis. Adv Parasitol. 2005;59:77–158. doi:10.1016/S0065-308X(05)59002-X.
9.
Feng Y, Ryan UM, Xiao L. Genetic Diversity and Population Structure of Cryptosporidium. Trends Parasitol. 2018;34(11):997–1011. doi:10.1016/j.pt.2018.07.009.
10.
Nader JL, Mathers TC, Ward BJ, et al. Evolutionary genomics of anthroponosis in Cryptosporidium. Nat Microbiol. 2019;4(5):826–836. doi:10.1038/s41564-019-0377-x.
11.
Widmer G, Carmena D, Kváč M, et al. Update on Cryptosporidium spp.: highlights from the Seventh International Giardia and Cryptosporidium Conference. Mise à jour sur Cryptosporidium spp.: Faits saillants de la Septième Conférence Internationale sur Giardia et Cryptosporidium. Parasite. 2020;27:14. doi:10.1051/parasite/2020011.
12.
Putignani L, Menichella D. Global distribution, public health and clinical impact of the protozoan pathogen cryptosporidium. Interdiscip Perspect Infect Dis. 2010;2010:753512. doi:10.1155/2010/753512.
13.
Centers for Disease Control and Prevention (CDC). CDC Yellow Book 2024: Health Information for International Travel. Oxford University Press; 2023.
14.
Golan Shaposhnik E, Abozaid S, Grossman T, et al. The Prevalence of Cryptosporidium among Children Hospitzed because of Gastrointestinal Symptoms and the Efficiency of Diagnostic Methods for Cryptosporidium. Am J Trop Med Hyg. 2019;101(1):160–163. doi:10.4269/ajtmh.19-0057.
15.
Fischer RT, Day JC, Wasserkrug H, et al. Complications of Cryptosporidium infection after pediatric liver transplantation: Diarrhea, rejection, and biliary disease. Pediatr Transplant. 2020;24(8):e13807. doi:10.1111/petr.13807.
16.
Hassan EM, Örmeci B, DeRosa MC, et al. A review of Cryptosporidium spp. and their detection in water. Water Sci Technol. 2021;83(1):1–25. doi:10.2166/wst.2020.515.
17.
Angel N Desai Cryptosporidiosis. JAMA. 2020;323(3):288. doi:10.1001/jama.2019.18691.
18.
Izadi S, Mohaghegh MA, Ghayour-Najafabadi Z, et al. Frequency and Molecular Identification of Cryptosporidium Species among Immunocompromised Patients Referred to Hospitals, Central Iran, 2015–16. Iran J Parasitol. 2020;15(1):31–39.
19.
Khan SM, Witola WH. Past, current, and potential treatments for cryptosporidiosis in humans and farm animals: A comprehensive review. Front Cell Infect Microbiol. 2023;13:1115522. doi:10.3389/fcimb.2023.1115522.
20.
Qin H, Chen Y, Wu Y, et al. Global prevalence of Cryptosporidium andersoni in dairy cattle: A systematic review and meta-analysis. Acta Trop. 2024;260:107427. doi:10.1016/j.actatropica.2024.107427.
21.
Lynch VD, Shaman J. Waterborne Infectious Diseases Associated with Exposure to Tropical Cyclonic Storms, United States, 1996–2018. Emerg Infect Dis. 2023;29(8):1548–1558. doi:10.3201/eid2908.221906.
22.
Khan SA, Khan I, Ali I, et al. Molecular detection of Cryptosporidium: an emerging parasite in different water sources of 2010 flood-affected district Nowshera, Pakistan [published correction appears in Arch Microbiol. 2022 Feb 4;204(3):161. doi:10.1007/s00203-021-02745-1]. Arch Microbiol. 2021;203(7):4397–4403. doi:10.1007/s00203-021-02419-y.
23.
Centers for Disease Control and Prevention (CDC). Early warning disease surveillance after a flood emergency – Pakistan, 2010. MMWR Morb Mortal Wkly Rep. 2012;61(49):1002–1007.
24.
Liu A, Gong B, Liu X, et al. A retrospective epidemiological analysis of human Cryptosporidium infection in China during the past three decades (1987–2018). PLoS Negl Trop Dis. 2020;14(3):e0008146. doi:10.1371/journal.pntd.0008146.
25.
Mac Kenzie WR, Hoxie NJ, Proctor ME, et al. A massive outbreak in Milwaukee of cryptosporidium infection transmitted through the public water supply [published correction appears in N Engl J Med 1994 Oct 13;331(15):1035]. N Engl J Med. 1994;331(3):161–167. doi:10.1056/NEJM199407213310304.
26.
Adeyemo FE, Singh G, Reddy P, et al. Efficiency of chlorine and UV in the inactivation of Cryptosporidium and Giardia in wastewater. PLoS One. 2019;14(5):e0216040. doi:10.1371/journal.pone.0216040.
27.
Rennecker JL, AM. Driedger SAA, et al. Synergy in sequential inactivation of Cryptosporidium parvum with ozone/free chlorine and ozone/monochloramine, Water Res. 2000;34(17):4121–4130. doi:10.1016/S0043-1354(00)00188-3.
28.
Reinoso R, Bécares E. Environmental inactivation of Cryptosporidium parvum oocysts in waste stabilization ponds. Microb Ecol. 2008;56(4):585–592. doi:10.1007/s00248-008-9378-7.
29.
Abeledo-Lameiro MJ, Ares-Mazás E, Goméz-Couso H. Use of ultrasound irradiation to inactivate Cryptosporidium parvum oocysts in effluents from municipal wastewater treatment plants. Ultrason Sonochem. 2018;48:118–126. doi:10.1016/j.ultsonch.2018.05.013.
30.
Ahmed M. Intestinal Parasitic Infections in 2023. Gastroenterology Res. 2023;16(3):127–140. doi:10.14740/gr1622.
31.
Fox LM, Saravolatz LD. Nitazoxanide: a new thiazolide antiparasitic agent. Clin Infect Dis. 2005;40(8):1173–1180. doi:10.1086/428839.
32.
Checkley W, White AC Jr, Jaganath D, et al. A review of the global burden, novel diagnostics, therapeutics, and vaccine targets for Cryptosporidium. Lancet Infect. Dis. 2015;15(1):85–94. doi:10.1016/S1473-3099(14)70772-8.
33.
Ali M, Xu C, Wang J et al. Emerging therapeutic avenues against Cryptosporidium: A comprehensive review. Vet Parasitol. 2024;331:110279. doi:10.1016/j.vetpar.2024.110279.
34.
Razzolini MTP, Breternitz BS, Kuchkarian B, et al. Cryptosporidium and Giardia in urban wastewater: A challenge to overcome. Environ Pollut. 2020;257(113545). https://doi.org/10.1016/j.envp....
35.
Peñuelas Martinez M, Carmena D, Guzmán Herrador BR, et al. Marked increase in cryptosporidiosis cases, Spain, 2023. Euro Surveill. 2024;29(28):2300733. doi:10.2807/1560-7917.ES.2024.29.28.2300733.
36.
Campbell SM, Pettersen FO, Brekke H, et al. Transition to PCR diagnosis of cryptosporidiosis and giardiasis in the Norwegian healthcare system: could the increase in reported cases be due to higher sensitivity or a change in the testing algorithm? Eur J Clin Microbiol Infect Dis. 2022;41(5):835–839. doi:10.1007/s10096-022-04426-3.
37.
Loeck BK, Pedati C, Iwen PC, et al. Genotyping and Subtyping Cryptosporidium To Identify Risk Factors and Transmission Patterns – Nebraska, 2015–2017. MMWR Morb Mortal Wkly Rep. 2020;69(12):335–338. doi:10.15585/mmwr.mm6912a4.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.