REVIEW PAPER
Impact of the Anti-Vaccination Movement on the health of children and society
1
Wydział Lekarski, Uniwersytet Medyczny im. Piastów Śląskich we Wrocławiu
2
Wydział Lekarski, Uniwersytet Opolski, Polska
3
Wojewódzki Szpital Specjalistyczny we Wrocławiu
These authors had equal contribution to this work
Med Srod. 2025;28(3):115-119
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The Anti-Vaccination Movement has become a significant concern for public health, challenging scientific consensus on vaccine safety and effectiveness, and contributing to declining vaccination rates. The review discusses the consequences of the movement for the health of children and society, with emphasis on psychological factors driving vaccine hesitancy, and presents strategies to mitigate its negative impact.
Brief description of the state of knowledge:
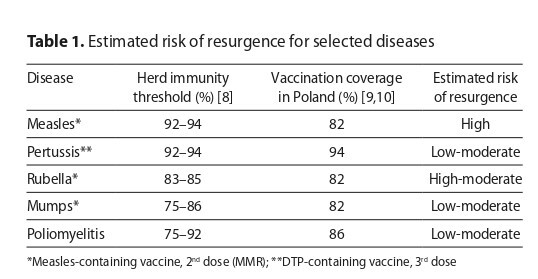
Medically, the movement has led to a resurgence of preventable diseases such as measles and pertussis. Reduced herd immunity endangers children too young or medically unable to receive vaccines and increases healthcare burdens. Socially, rapidly spreading misinformation, especially on social media, influences public perception more than scientific facts and undermines trust in healthcare professionals. Psychologically, vaccine refusal is fuelled by cognitive biases, fear, conspiracy thinking, and emotional narratives, which often outweigh data-based communication. These mechanisms explain the persistence of false beliefs despite factual corrections
Summary:
The movement poses a complex threat to both individual health and trust in science. Combatting it requires consistent medical guidance, strong public health messaging, and building lasting trust in healthcare providers. Effective strategies include the 3Cs model (confidence, convenience, complacency) and the CASE (corroborate, about me, science, explain) approach. Success depends on addressing emotional and cognitive barriers through respectful, empathetic communication and evidence-based advocacy
The Anti-Vaccination Movement has become a significant concern for public health, challenging scientific consensus on vaccine safety and effectiveness, and contributing to declining vaccination rates. The review discusses the consequences of the movement for the health of children and society, with emphasis on psychological factors driving vaccine hesitancy, and presents strategies to mitigate its negative impact.
Brief description of the state of knowledge:
Medically, the movement has led to a resurgence of preventable diseases such as measles and pertussis. Reduced herd immunity endangers children too young or medically unable to receive vaccines and increases healthcare burdens. Socially, rapidly spreading misinformation, especially on social media, influences public perception more than scientific facts and undermines trust in healthcare professionals. Psychologically, vaccine refusal is fuelled by cognitive biases, fear, conspiracy thinking, and emotional narratives, which often outweigh data-based communication. These mechanisms explain the persistence of false beliefs despite factual corrections
Summary:
The movement poses a complex threat to both individual health and trust in science. Combatting it requires consistent medical guidance, strong public health messaging, and building lasting trust in healthcare providers. Effective strategies include the 3Cs model (confidence, convenience, complacency) and the CASE (corroborate, about me, science, explain) approach. Success depends on addressing emotional and cognitive barriers through respectful, empathetic communication and evidence-based advocacy
REFERENCES (32)
1.
Ortiz-Sánchez E, Velando-Soriano A, Pradas-Hernández L, et al. Analysis of the Anti-Vaccine Movement in Social Networks: A Systematic Review. Int J Environ Res Public Health. 2020;17(15):5394. https://doi.org/10.3390/ijerph....
2.
Benoit S, Mauldin R. The “anti-vax” movement: a quantitative report on vaccine beliefs and knowledge across social media. BMC Public Health. 2021;17;21(1):2106. https://doi.org/10.1186/s12889....
3.
Borba R, Vidal V, Moreira L. The re-emergency and persistence of vaccine preventable diseases. An Acad Bras Ciênc. 2015;25;87:1311–1322. https://doi.org/10.1590/0001-3....
4.
Plans-Rubió P. Measles Vaccination Coverage and Anti-Measles Herd Immunity Levels in the World and WHO Regions Worsened from 2019 to 2023. Vaccines. 2025;13(2):157. https://doi.org/10.3390/vaccin...
5.
Jagieła K, Walowska D, Klocek W, et al. Evaluation of parents’ knowledge of mandatory and recommended vaccinations for children in the city of Zielona Góra, taking into account medical and non-medical professions. Pol J Public Health. 2023;133:22–26. https://doi.org/10.12923/2083-....
6.
Dubé E, Vivion M, MacDonald N. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: influence, impact and implications. Exp Rev Vaccin. 2015;14(1):99–117. https://doi.org/10.1586/147605....
7.
Mrukowicz J. Mózg w sidłach mikrobów czyli czego nie widzimy dzięki szczepieniom ochronnym. Wszechświat. 2011;112(4–6):84–93.
8.
WHO and UNICEF. WHO/UNICEF Estimates of National Immunization Coverage, 2024 Revision (completed 15 July 2025). https:// worldhealthorg.shinyapps.io/wuenic-trends/ (access: 2025.08.13).
9.
WHO. WHO Immunization Data portal – Detail Page. Immunization Data. https://immunizationdata.who.i... (access: 2025.08.13).
10.
Vignesh R, Shankar E, Velu V, et al. Is Herd Immunity Against SARSCoV- 2 a Silver Lining? Front Immunol. 2020;11:586781. https://doi.org/10.3389/fimmu.....
11.
Seremak-Mrozikiewicz A, Nitsch-Osuch A, Czajkowski K, et al. Guidelines of the Polish Society of Gynecologists and Obstetricians, the Polish Society for Vaccinology, and the Polish Society for Family Medicine on vaccinating women with reproductive plans and pregnant or breastfeeding women. Ginekol Pol. 2023;94(8):670–682. https://doi.org/10.5603/gpl.95....
12.
Farrenkopf P. The Cost of Ignoring Vaccines. Yale J Biol Med. 2022;30;95(2):265–269.
13.
Gallegos M, de Castro Pecanha V, Caycho-Rodríguez T. Anti-vax: the history of a scientific problem. J Public Health. 2023;45(1):e140–141. https://doi.org/10.1093/pubmed....
14.
Novilla M, Lelinneth B, et al. Why Parents Say No to Having Their Children Vaccinated against Measles: A Systematic Review of the Social Determinants of Parental Perceptions on MMR Vaccine Hesitancy. Vaccines. 2023;11(5):926. https://doi.org/10.3390/vaccin....
15.
Skea Z, Entwistle V, Watt I, et al. ‘Avoiding harm to others’ considerations in relation to parental measles, mumps and rubella (MMR) vaccination discussions – An analysis of an online chat forum. Soc Sci Med. 2008;67(9):1382–1390. https://doi.org/10.1016/j.socs....
16.
Sallam M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines. 2021;9(2):160. https://doi.org/10.3390/vaccin....
17.
Lee S, Sun J, Jang S, et al. Misinformation of COVID-19 vaccines and vaccine hesitancy. Sci Rep. 2022;12(1):13681. https://doi.org/10.1038/s41598....
18.
Arambul N, Sraboni S, Chukwunweike J, et al. Exploring the Association between Trust in Healthcare Entities and Exposure to Emerging Health Misinformation in Nebraska: A Pilot Study. Proceedings of the Human Factors and Ergonomics Society Annual Meeting. 2023;67(1):1731–1734. https://doi.org/10.1177/216950....
19.
Corinti F, Pontillo D, Giansanti D. COVID-19 and the Infodemic: An Overview of the Role and Impact of Social Media, the Evolution of Medical Knowledge, and Emerging Problems. Healthcare. 2022;10(4):732. https://doi.org/10.3390healthc....
20.
Loomba S, de Figueiredo A, Piatek S, et al. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat Hum Behav. 2021;5(3):337–348. https://doi.org/10.1038/s41562....
21.
Skafle I, Nordahl-Hansen A, Quintana D, et al. Misinformation About COVID-19 Vaccines on Social Media: Rapid Review. J Med Internet Res. 2022;24(8):e37367. https://doi.org/10.2196/37367.
22.
Silver D, Kim Y, McNeill E, et al. Association between COVID-19 vaccine hesitancy and trust in the medical profession and public health officials. Prev Med. 2022;164:107311. https://doi.org/10.1016/j.ypme...
23.
Winter K, Pummerer L, Hornsey M, et al. Pro-vaccination subjective norms moderate the relationship between conspiracy mentality and vaccination intentions. Br J Health Psychol. 2022;27(2):390–405. https:// doi.org/10.1111/bjhp.12550.
24.
Enders A, Uscinski J, Klofstad C, et al. On the relationship between conspiracy theory beliefs, misinformation, and vaccine hesitancy. PLoS One. 2022;17(10):e0276082. https://doi.org/10.1371/journa....
25.
Kwek A, Peh L, Tan J, et al. Distractions, analytical thinking and falling for fake news: A survey of psychological factors. Humanit Soc Sci Commun. 2023;10(1):1–12. https://doi.org/10.1057/s41599....
26.
Cassam Q. Conspiracy Theories. Society. 2023;60(2):190–199. https:// doi.org/10.1007/s12115-023-00816-1.
27.
Dubé È, Ward J, Verger P, et al. Vaccine Hesitancy, Acceptance, and Anti-Vaccination: Trends and Future Prospects for Public Health. Annu Rev Public Health. 2021;42:175–191. https://doi.org/10.1146/annure....
28.
Gianfredi V, Moretti M, Lopalco P. Countering vaccine hesitancy through immunization information systems, a narrative review. Hum Vaccin Immunother. 2019;15(11):2508–2526. https://doi.org/10.1080/216455....
29.
Leask J, Kinnersley P, Jackson C, et al. Communicating with parents about vaccination: a framework for health professionals. BMC Pediatrics. 2012;12(1):154. https://doi.org/10.1186/1471-2....
30.
National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Global Health, et al. The Critical Public Health Value of Vaccines: Tackling Issues of Access and Hesitancy. Proceedings of a Workshop; 2020 Aug 17–20; Washington (DC), USA. National Academies Press; 2021.
31.
Jacobson R, Sauver J, Rutten L. Vaccine Hesitancy. Mayo Clinic Proceedings. 2015;90(11):1562–1568.
32.
Jacobson R, Van Etta L, Bahta L. The C.A.S.E. approach: guidance for talking to vaccine-hesitant parents. Minn Med. 2013;96(4):49–50.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.