Online first
Bieżący numer
O czasopiśmie
Archiwum
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Bazy indeksacyjne
Komitet Redakcyjny
Recenzenci
2024
2023
2022
2021
2020
2019
2018
Kontakt
Klauzula przetwarzania danych osobowych (RODO)
PRACA POGLĄDOWA
Zmiany hormonalne w przebiegu choroby otyłościowej
1
Wojewódzki Szpital Specjalistyczny we Wrocławiu, Ośrodek Badawczo-Rozwojowy, Wrocław, Polska
2
Uniwersytecki Szpital Kliniczny we Wrocławiu, Polska
3
Dolnośląski Szpital Specjalistyczny im. T. Marciniaka – Centrum Medycyny Ratunkowej, Wrocław, Polska
Autor do korespondencji
Marcin Maciej Dereziński
Wojewódzki Szpital Specjalistyczny we Wrocławiu Ośrodek Badawczo-Rozwojowy ul. H. M. Kamieńskiego 73a 51-124 Wrocław, Kręta 21/46, 50-233, Wrocław, Polska
Wojewódzki Szpital Specjalistyczny we Wrocławiu Ośrodek Badawczo-Rozwojowy ul. H. M. Kamieńskiego 73a 51-124 Wrocław, Kręta 21/46, 50-233, Wrocław, Polska
Med Srod. 2023;26(1-2):20-25
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
Otyłość jest środowiskową chorobą przewlekłą, której znaczenie w zdrowiu publicznym stale rośnie. Tkanka tłuszczowa wykazuje aktywność hormonalną, a produkowane przez nią substancje, zwane adipokinami, biorą udział m.in. w regulacji podaży energetycznej oraz magazynowaniu energii. Ponadto wiele badań wskazuje na wpływ poziomu tkanki tłuszczowej i otyłości na aktywność innych hormonów produkowanych w organizmie człowieka. Celem niniejszej pracy jest przegląd dostępnej literatury na temat hormonów produkowanych przez tkankę tłuszczową oraz innych wybranych hormonów z nią związanych i podsumowanie wiedzy dotyczącej zależności pomiędzy nimi.
Opis stanu wiedzy:
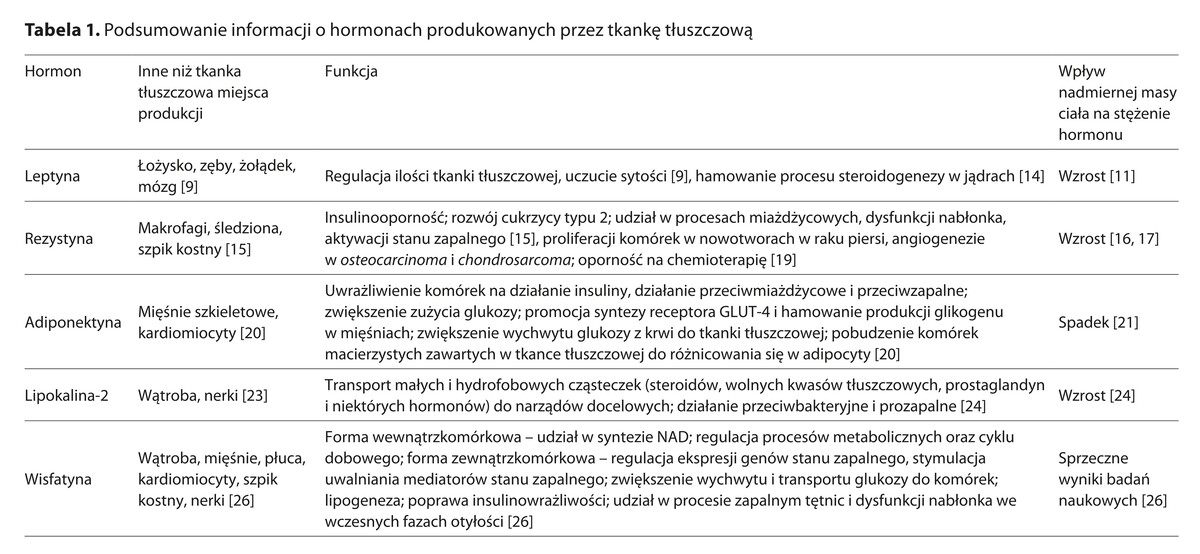
Leptyna jako plejotropowy hormon reguluje ilość tkanki tłuszczowej w organizmie i odpowiada m.in. za uczucie sytości. Rezystyna jest jednym z kluczowych hormonów prowadzących do rozwoju insulinooporności. Adiponektyna uwrażliwia komórki na działanie insuliny, działa przeciwmiażdżycowo, a także ma właściwości przeciwzapalne. Lipokalina na właściwości prozapalne. Tkanka tłuszczowa wpływa na stężenia hormonów tarczycy, prolaktyny, hormonów płciowych oraz na układ renina–angiotensyna–aldosteron (RAA).
Podsumowanie:
Rolą tkanki tłuszczowej – poza magazynowaniem energii – jest m.in. wydzielanie adipokin. Wśród nich należy wymienić m.in. leptynę, rezystynę, adiponektynę oraz wisfatynę. Modyfikują one metabolizm tkanki tłuszczowej, regulują uczucie sytości, rozwój insulinooporności i procesy miażdzycowe. Ponadto wykazano wpływ części z nich na ryzyko rozwoju cukrzycy i chorób sercowo-naczyniowych. Należy zaznaczyć, że rola tkanki tłuszczowej w gospodarce hormonalnej organizmu jest tylko częściowo poznana, ale jej zrozumienie może pomóc w skuteczniejszym leczeniu otyłości.
Otyłość jest środowiskową chorobą przewlekłą, której znaczenie w zdrowiu publicznym stale rośnie. Tkanka tłuszczowa wykazuje aktywność hormonalną, a produkowane przez nią substancje, zwane adipokinami, biorą udział m.in. w regulacji podaży energetycznej oraz magazynowaniu energii. Ponadto wiele badań wskazuje na wpływ poziomu tkanki tłuszczowej i otyłości na aktywność innych hormonów produkowanych w organizmie człowieka. Celem niniejszej pracy jest przegląd dostępnej literatury na temat hormonów produkowanych przez tkankę tłuszczową oraz innych wybranych hormonów z nią związanych i podsumowanie wiedzy dotyczącej zależności pomiędzy nimi.
Opis stanu wiedzy:
Leptyna jako plejotropowy hormon reguluje ilość tkanki tłuszczowej w organizmie i odpowiada m.in. za uczucie sytości. Rezystyna jest jednym z kluczowych hormonów prowadzących do rozwoju insulinooporności. Adiponektyna uwrażliwia komórki na działanie insuliny, działa przeciwmiażdżycowo, a także ma właściwości przeciwzapalne. Lipokalina na właściwości prozapalne. Tkanka tłuszczowa wpływa na stężenia hormonów tarczycy, prolaktyny, hormonów płciowych oraz na układ renina–angiotensyna–aldosteron (RAA).
Podsumowanie:
Rolą tkanki tłuszczowej – poza magazynowaniem energii – jest m.in. wydzielanie adipokin. Wśród nich należy wymienić m.in. leptynę, rezystynę, adiponektynę oraz wisfatynę. Modyfikują one metabolizm tkanki tłuszczowej, regulują uczucie sytości, rozwój insulinooporności i procesy miażdzycowe. Ponadto wykazano wpływ części z nich na ryzyko rozwoju cukrzycy i chorób sercowo-naczyniowych. Należy zaznaczyć, że rola tkanki tłuszczowej w gospodarce hormonalnej organizmu jest tylko częściowo poznana, ale jej zrozumienie może pomóc w skuteczniejszym leczeniu otyłości.
Introduction and objective:
Obesity is an environmental chronic disease and its significance in public health is constantly increasing. Adipose tissue exhibits hormonal activity and the substances it produces, called adipokines play a role in the regulation of energy supply and energy storage, among other functions. Moreover, numerous studies indicate a connection between the level of adipose tissue, obesity and activity of other hormones produced in the human body. The aim of this study is to review the available literature on hormones produced by adipose tissue, as well as other selected hormones associated with it, and to summarize knowledge regarding the relationships between them.
Brief description of the state of knowledge:
Leptin, as a pleiotropic hormone, regulates the amount of adipose tissue in the body and is responsible, among other things, for the feeling of satiety. Resistin is one of the key hormones leading to the development of insulin resistance. Adiponectin sensitizes cells to the action of insulin, has anti-atherosclerotic properties and also exhibits anti-inflammatory properties. Lipocalin 2 has pro-inflammatory properties. Adipose tissue affects the levels of thyroid hormones, prolactin, sex hormones and influences the renin-angiotensin-aldosterone system (RAAS).
Summary:
In addition to energy storage, adipose tissue secretes adipokines. Most important are leptin, resistin, adiponectin, and visfatin. They modulate metabolism of adipose tissue, regulate the feeling of satiety, insulin resistance and atherosclerotic processes. Furthermore, their impact on the risk of developing diabetes and cardiovascular diseases has been demonstrated. It should be noted that the role of adipose tissue in the hormonal regulation of the body is only partially understood, but understanding it may contribute to more effective treatment of obesity.
Obesity is an environmental chronic disease and its significance in public health is constantly increasing. Adipose tissue exhibits hormonal activity and the substances it produces, called adipokines play a role in the regulation of energy supply and energy storage, among other functions. Moreover, numerous studies indicate a connection between the level of adipose tissue, obesity and activity of other hormones produced in the human body. The aim of this study is to review the available literature on hormones produced by adipose tissue, as well as other selected hormones associated with it, and to summarize knowledge regarding the relationships between them.
Brief description of the state of knowledge:
Leptin, as a pleiotropic hormone, regulates the amount of adipose tissue in the body and is responsible, among other things, for the feeling of satiety. Resistin is one of the key hormones leading to the development of insulin resistance. Adiponectin sensitizes cells to the action of insulin, has anti-atherosclerotic properties and also exhibits anti-inflammatory properties. Lipocalin 2 has pro-inflammatory properties. Adipose tissue affects the levels of thyroid hormones, prolactin, sex hormones and influences the renin-angiotensin-aldosterone system (RAAS).
Summary:
In addition to energy storage, adipose tissue secretes adipokines. Most important are leptin, resistin, adiponectin, and visfatin. They modulate metabolism of adipose tissue, regulate the feeling of satiety, insulin resistance and atherosclerotic processes. Furthermore, their impact on the risk of developing diabetes and cardiovascular diseases has been demonstrated. It should be noted that the role of adipose tissue in the hormonal regulation of the body is only partially understood, but understanding it may contribute to more effective treatment of obesity.
REFERENCJE (51)
1.
Nuttall FQ. Body mass index: Obesity, BMI, and health: A critical review. Nutrition Today. 2015;50(3):117–128.
2.
Pi-Sunyer X. The medical risks of obesity. Postgrad Med. 2009;121(6):21–33.
3.
Coelho M, Oliveira T, Fernandes R. Biochemistry of adipose tissue: An endocrine organ. Archiv Med Sci. 2013;9(2):191–200.
4.
Wójcik B, Górski J. Brown adipose tissue in adult humans: distribution and function. Endokrynol. Otyłość. Zaburzenia Przemiany Materii. 2011;7(1):34–40.
5.
Dongre UJ. Adipokines in Insulin Resistance: Current Updates. Biosci Biotechnol Res Asia. 2021;18(2):357–366.
6.
Lin X, Li H. Obesity: Epidemiology, Pathophysiology, and Therapeutics. Frontiers in Endocrinology. 2021;12. doi:10.3389/fendo.2021.706978.
7.
Gao R, Zhu C, Li H, et al. Dysbiosis Signatures of Gut Microbiota Along the Sequence from Healthy, Young Patients to Those with Overweight and Obesity. Obesity. 2018;26(2):351–361.
8.
Breton J, Galmiche M, Déchelotte P. Dysbiotic Gut Bacteria in Obesity: An Overview of the Metabolic Mechanisms and Therapeutic Perspectives of Next-Generation Probiotics. Microorganisms. 2022;10(2). doi:10.3390/microorganisms10020452.
9.
Obradovic M, Sudar-Milovanovic E, Soskic S, et al. Leptin and Obesity: Role and Clinical Implication. Front Endocrinol. 2021;12. doi:10.3389/fendo.2021.585887.
10.
Kelesidis T, Kelesidis I, Chou S, et al. Narrative review: The role of leptin in human physiology: Emerging clinical applications. Ann Intern Med. 2010;152(2):93–100.
11.
Kumar R, Mal K, Razaq MK, et al. Association of Leptin With Obesity and Insulin Resistance. Cureus. 2020. doi:10.7759/cureus.12178.
12.
Park HK, Ahima RS. Physiology of leptin: energy homeostasis, neuroendocrine function and metabolism. Metabol Clin Experimental. 2015;64(1):24–34.
13.
Izquierdo AG, Crujeiras AB, Casanueva FF, et al. Leptin, obesity, and leptin resistance: where are we 25 years later? Nutrients. 2019;11(11). doi:10.3390/nu11112704.
14.
Fernandes Negris Lima T, Nackeeran S, Rakitina E, et al. Association of Leptin with Total and Free Testosterone: Results from the National Health and Nutrition Examination Surveys. Androgens. 2020;1(1):94–100.
15.
Jamaluddin MS, Weakley SM, Yao Q, et al. Themed Section: Fat and Vascular Responsiveness Resistin: functional roles and therapeutic considerations for cardiovascular disease. British J Pharmacol. 2012 Feb;165(3):622–32. https://doi.org/10.1111/j.1476....
16.
Nieva-Vazquez A, Pérez-Fuentes R, Torres-Rasgado E, et al. Serum resistin levels are associated with adiposity and insulin sensitivity in obese hispanic subjects. Metab Syndr Relat Disord. 2014;12(2):143–148.
17.
Azuma K, Katsukawa F, Oguchi S, et al. Correlation between Serum Resistin Level and Adiposity in Obese Individuals. Obes Res. 2003 Aug;11(8):997–1001.
18.
Chen BH, Song Y, Ding EL, et al. Circulating levels of resistin and risk of type 2 diabetes in men and women: Results from two prospective cohorts. Diabetes Care. 2009;32(2):329–334.
19.
Deb A, Deshmukh B, Ramteke P, et al. Resistin: A journey from metabolism to cancer. Translational Oncology. 2021;14(10). doi:10.1016/j.tranon.2021.101178.
20.
Achari AE, Jain SK. Adiponectin, a therapeutic target for obesity, diabetes, and endothelial dysfunction. Intern J Molecular Sci. 2017;18(6). doi:10.3390/ijms18061321.
21.
Diep Nguyen T. Adiponectin: Role in physiology and pathophysiology. Int J Prev Med. 2020;11(1):136.
22.
El-Mesallamy HO, Hamdy NM, Salman TM, et al. Adiponectin and sE-selectin concentrations in relation to inflammation in obese type 2 diabetic patients with coronary heart disease. Angiology. 2012;63(2):96–102.
23.
Jaberi S Al, Cohen A, D’Souza C, et al. Lipocalin-2: Structure, function, distribution and role in metabolic disorders. Biomed Pharmacotherapy. 2021;142. doi:10.1016/j.biopha.2021.112002.
24.
Huang Y, Yang Z, Ye Z, et al. Lipocalin-2, glucose metabolism and chronic low-grade systemic inflammation in Chinese people. Cardiovasc Diabetol. 2012;11. doi:10.1186/1475-2840-11-11.
25.
Dongre UJ. Adipokines in Insulin Resistance: Current Updates. Biosci Biotechnol Res Asia. 2021;18(2):357–36.
26.
Dakroub A, A Nasser S, Younis N, et al. Visfatin: A Possible Role in Cardiovasculo-Metabolic Disorders. Cells. 2020;9(11). doi:10.3390/cells9112444.
27.
Cabandugama PK, Gardner MJ, Sowers JR. The Renin Angiotensin Aldosterone System in Obesity and Hypertension: Roles in the Cardiorenal Metabolic Syndrome. Med Clin North Am. 2017;101(1):129–137.
28.
Kern PA, Saghizadeh M, Ong JM, et al. The expression of tumor necrosis factor in human adipose tissue: Regulation by obesity, weight loss, and relationship to lipoprotein lipase. J Clin Investigation. 1995;95(5):2111–2119.
29.
Kras KM, Hausman DB, Martin RJ. Tumor Necrosis Factor-Stimulates Cell Proliferation in Adipose Tissue-Derived Stromal-Vascular Cell Culture: Promotion of Adipose Tissue Expansion by Paracrine Growth Factors. Obes Res. 2000 Mar;8(2):186–93. doi:10.1038/oby.2000.20.
30.
Cawthorn WP, Sethi JK. TNF-? and adipocyte biology. FEBS Letters. 2008;582(1):117–131. https://doi.org/10.1016/j.febs....
31.
Patsalos O, Dalton B, Leppanen J, et al. Impact of TNF-a inhibitors on body weight and BMI: A systematic review and meta-analysis. Frontn Pharmacol. 2020;11. doi:10.3389/fphar.2020.00481.
32.
Ye J. Mechanisms of insulin resistance in obesity. Front Med China. 2013;7(1):14–24.
33.
Kwon H, Pessin JE. Adipokines mediate inflammation and insulin resistance. Front Endocrinol. 2013;4(JUN). doi:10.3389/fendo.2013.00071.
34.
Nicholson T, Church C, Baker DJ, et al. The role of adipokines in skeletal muscle inflammation and insulin sensitivity. J Inflammation (United Kingdom). 2018;15(1). doi:10.1186/s12950-018-0185-8.
35.
Freeman AM, Pennings N. Insulin Resistance. 2022 Sep 20. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 29939616.
36.
Fu J, Zhang L, An Y, et al. Association between body mass index and thyroid function in euthyroid chinese adults. Med Sci Monitor. 2021;27. doi:10.12659/MSM.930865.
37.
Laurberg P, Knudsen N, Andersen S, et al. Thyroid Function and Obesity. Eur Thyroid J. 2012;1(3):159–167.
38.
Xu R, Huang F, Zhang S, et al. Thyroid function, body mass index, and metabolic risk markers in euthyroid adults: A cohort study. BMC Endocr Disord. 2019;19(1). doi:10.1186/s12902-019-0383-2.
39.
Walczak K, Sieminska L. Obesity and thyroid axis. Inter J Environ Res Public Health. 2021;18(18). doi:10.3390/ijerph18189434.
40.
Song RH, Wang B, Yao QM, et al. The Impact of Obesity on Thyroid Autoimmunity and Dysfunction: A Systematic Review and Meta-Analysis. Front Immunol. 2019;10. doi:10.3389/fimmu.2019.02349.
41.
Sanyal D, Raychaudhuri M. Hypothyroidism and obesity: An intriguing link. Indian J Endocrinol Metabol. 2016;20(4):554–557.
42.
Abraham SB, Rubino D, Sinaii N, et al. Cortisol, obesity, and the metabolic syndrome: A cross-sectional study of obese subjects and review of the literature. Obesity. 2013;21(1):E105–E117.
43.
van der Valk ES, Savas M, van Rossum EFC. Stress and Obesity: Are There More Susceptible Individuals? Current obesity reports. 2018;7(2):193–203.
44.
Pirchio R, Graziadio C, Colao A, et al. Metabolic effects of prolactin. Front Endocrinol. 2022;13. doi:10.3389/fendo.2022.1015520.
45.
Holt RIG, Barnett AH, Bailey CJ. Bromocriptine: Old drug, new formulation and new indication. Diabetes Obesity Metab. 2010;12(12):1048–1057.
46.
Ernst B, Thurnheer M, Schultes B. Basal serum prolactin levels in obesity-unrelated to parameters of the metabolic syndrome and unchanged after massive weight loss. Obes Surg. 2009;19(8):1159–1162.
47.
Liu J, Wang Q, Zhang L, et al. Increased Prolactin is an Adaptive Response to Protect Against Metabolic Disorders in Obesity. Endocr Pract. 2021;27(7):728–735.
48.
Liu J, Zhang L, Fu J, et al. Circulating prolactin level is increased in metabolically healthy obesity. Endocr Connect. 2021;10(4):484–491.
49.
Freeman EW, Sammel MD, Lin H, et al. Obesity and reproductive hormone levels in the transition to menopause. Menopause. 2010;17(4):718–726.
50.
Saad F, Aversa A, Isidori AM, et al. Testosterone as Potential Effective Therapy in Treatment of Obesity in Men with Testosterone Deficiency: A Review. Curr Diabetes Rev. 2012;8(2):131–143. doi:10.2174/157339912799424573.
51.
Eriksson J, Haring R, Grarup N, et al. Causal relationship between obesity and serum testosterone status in men: A bidirectional mendelian randomization analysis. PLoS One. 2017;12(4). doi:10.1371/journal.pone.0176277.
Udostępnij
ARTYKUŁ POWIĄZANY
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.