Online first
Bieżący numer
O czasopiśmie
Archiwum
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Bazy indeksacyjne
Komitet Redakcyjny
Recenzenci
2024
2023
2022
2021
2020
2019
2018
Kontakt
Klauzula przetwarzania danych osobowych (RODO)
PRACA POGLĄDOWA
Związek snu z otyłością – przegląd literatury
1
Oncology Department, Dr. Jan Jonston Regional Multispecialty Hospital, Leszno, Poland
2
Internal Medicine and Cardiology Department with Internal Medicine and Cardiology Intensive Care Unit, Provincial Hospital, Poznań, Poland
Autor do korespondencji
Józef Muszyński
Oddział onkologiczny, Wojewódzki Szpital Wielospecjalistyczny im. dr. Jana Jonstona w Lesznie, Polska
Oddział onkologiczny, Wojewódzki Szpital Wielospecjalistyczny im. dr. Jana Jonstona w Lesznie, Polska
Med Srod. 2025;28(1):24-28
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
Otyłość to stan, w którym dochodzi do nadmiernego gromadzenia się tkanki tłuszczowej, wynikający z braku równowagi między poborem energii a jej wydatkowaniem. Jest to istotny problem zdrowotny, który może negatywnie wpływać na jakość snu. Jednocześnie zaburzenia snu, takie jak jego niedobór lub niska jakość, mogą sprzyjać rozwojowi otyłości, tworząc błędne koło. Artykuł ma na celu zebranie i podsumowanie najnowszych odkryć naukowych dotyczących związku między zaburzeniami snu a otyłością.
Opis stanu wiedzy:
Źródła zostały pozyskane za pośrednictwem baz PubMed oraz Google Scholar, z wykorzystaniem słów kluczowych: „otyłość”, „bezsenność”, „zaburzenia snu”. Przegląd literatury przeprowadzono w okresie od października 2024 roku do stycznia 2025 roku. Obecnie nie ma jasnego konsensusu co do tego, czy to otyłość prowadzi do zaburzeń snu, czy też zaburzenia snu sprzyjają rozwojowi otyłości. Wraz ze zmianami populacyjnymi obserwuje się coraz krótszy czas trwania snu. Otyłość może upośledzać wydzielanie greliny i leptyny oraz zaburzać produkcję melatoniny. Dodatkowo predysponuje do występowania bezdechu sennego, który przyczynia się do zaburzeń snu. Badania wykazały związek między różnymi porami snu a ryzykiem otyłości. Osoby, które śpią za krótko, mają trudności z redukcją masy ciała.
Podsumowanie:
Otyłość to poważny problem cywilizacyjny, który może prowadzić do wielu zaburzeń. Badania wskazują na jej wpływ na zaburzenia snu, choć wciąż nie ma jednoznacznej zgody co do tego, czy zależność ta działa również w drugą stronę. Wiadomo jednak, że otyłość wpływa na zaburzenia hormonalne i anatomiczne, które mogą sprzyjać jej dalszemu rozwojowi. Jednocześnie nieregularne pory i niedobór snu wiąże się ze zwiększonym ryzykiem otyłości. Sugeruje się, że edukacja, lepsze zarządzanie snem i odpowiednia dieta mogą poprawić jakość snu, a tym samym wspomóc leczenie otyłości.
Otyłość to stan, w którym dochodzi do nadmiernego gromadzenia się tkanki tłuszczowej, wynikający z braku równowagi między poborem energii a jej wydatkowaniem. Jest to istotny problem zdrowotny, który może negatywnie wpływać na jakość snu. Jednocześnie zaburzenia snu, takie jak jego niedobór lub niska jakość, mogą sprzyjać rozwojowi otyłości, tworząc błędne koło. Artykuł ma na celu zebranie i podsumowanie najnowszych odkryć naukowych dotyczących związku między zaburzeniami snu a otyłością.
Opis stanu wiedzy:
Źródła zostały pozyskane za pośrednictwem baz PubMed oraz Google Scholar, z wykorzystaniem słów kluczowych: „otyłość”, „bezsenność”, „zaburzenia snu”. Przegląd literatury przeprowadzono w okresie od października 2024 roku do stycznia 2025 roku. Obecnie nie ma jasnego konsensusu co do tego, czy to otyłość prowadzi do zaburzeń snu, czy też zaburzenia snu sprzyjają rozwojowi otyłości. Wraz ze zmianami populacyjnymi obserwuje się coraz krótszy czas trwania snu. Otyłość może upośledzać wydzielanie greliny i leptyny oraz zaburzać produkcję melatoniny. Dodatkowo predysponuje do występowania bezdechu sennego, który przyczynia się do zaburzeń snu. Badania wykazały związek między różnymi porami snu a ryzykiem otyłości. Osoby, które śpią za krótko, mają trudności z redukcją masy ciała.
Podsumowanie:
Otyłość to poważny problem cywilizacyjny, który może prowadzić do wielu zaburzeń. Badania wskazują na jej wpływ na zaburzenia snu, choć wciąż nie ma jednoznacznej zgody co do tego, czy zależność ta działa również w drugą stronę. Wiadomo jednak, że otyłość wpływa na zaburzenia hormonalne i anatomiczne, które mogą sprzyjać jej dalszemu rozwojowi. Jednocześnie nieregularne pory i niedobór snu wiąże się ze zwiększonym ryzykiem otyłości. Sugeruje się, że edukacja, lepsze zarządzanie snem i odpowiednia dieta mogą poprawić jakość snu, a tym samym wspomóc leczenie otyłości.
Introduction and objective:
Obesity is a condition in which there is an excessive accumulation of body fat, resulting from an imbalance between energy intake and energy expenditure. This is a significant health problem that can negatively affect the quality of sleep. At the same time, sleep disorders, such as sleep deficiency or poor quality sleep, can promote the development of obesity, creating a vicious cycle. The aim of the review is to collect and summarize recent scientific findings on the relationship between sleep disorders and obesity.
Abbreviated description of the state of knowledge:
Sources were obtained using PubMed and Google Scholar, using the key words: ‘obesity’, ‘insomnia’, ‘sleep disorders’. The review was conducted from October 2024 – January 2025. Currently, there is no clear consensus on whether it is obesity that leads to sleep disorders, or whether sleep disorders promote the development of obesity. With the change of lifestyle, a shorter and shorter sleep duration is observed. Obesity can impair the secretion of ghrelin and leptin, and interfere with melatonin production. Additionally, it predisposes to the occurrence of sleep apnea, which itself contributes to sleep disorders. Studies have shown a link between different bedtimes and obesity risk. People who sleep less, often have difficulty reducing weight.
Conclusions:
Obesity is a serious civilization problem that can lead to many disorders. Studies indicate its association with sleep disorders, although there is still no clear consensus on whether the relationship also works the other way round. What is known, however, is that obesity affects hormonal and anatomical disorders that can promote its further development. At the same time, an irregular sleep schedule is associated with an increased risk of obesity. It has been suggested that education, better sleep management, and an appropriate diet could improve sleep quality and thus support the treatment of obesity.
Obesity is a condition in which there is an excessive accumulation of body fat, resulting from an imbalance between energy intake and energy expenditure. This is a significant health problem that can negatively affect the quality of sleep. At the same time, sleep disorders, such as sleep deficiency or poor quality sleep, can promote the development of obesity, creating a vicious cycle. The aim of the review is to collect and summarize recent scientific findings on the relationship between sleep disorders and obesity.
Abbreviated description of the state of knowledge:
Sources were obtained using PubMed and Google Scholar, using the key words: ‘obesity’, ‘insomnia’, ‘sleep disorders’. The review was conducted from October 2024 – January 2025. Currently, there is no clear consensus on whether it is obesity that leads to sleep disorders, or whether sleep disorders promote the development of obesity. With the change of lifestyle, a shorter and shorter sleep duration is observed. Obesity can impair the secretion of ghrelin and leptin, and interfere with melatonin production. Additionally, it predisposes to the occurrence of sleep apnea, which itself contributes to sleep disorders. Studies have shown a link between different bedtimes and obesity risk. People who sleep less, often have difficulty reducing weight.
Conclusions:
Obesity is a serious civilization problem that can lead to many disorders. Studies indicate its association with sleep disorders, although there is still no clear consensus on whether the relationship also works the other way round. What is known, however, is that obesity affects hormonal and anatomical disorders that can promote its further development. At the same time, an irregular sleep schedule is associated with an increased risk of obesity. It has been suggested that education, better sleep management, and an appropriate diet could improve sleep quality and thus support the treatment of obesity.
REFERENCJE (38)
1.
Savulescu-Fiedler I, Mihalcea R, Dragosloveanu S, et al. The interplay between obesity and inflammation. Life. 2024 Jul 8;14(7):856.
2.
Han SH, Yee JY, Pyo JS. Impact of short sleep duration on the incidence of obesity and overweight among children and adolescents. Medicina. 2022 Aug 2;58(8):1037.
3.
Nittari G, Scuri S, Sagaro GG, et al. Epidemiology of obesity in children and adolescents. Teamwork in Healthcare. 2020 Sep 17;1:20.
4.
Pardak P, Filip R, Woliński J. The impact of sleep-disordered breathing on ghrelin, obestatin, and leptin profiles in patients with obesity or overweight. J Clin Med. 2022 Apr 5;11(7):2032.
5.
Hawes NJ, Wiggins AT, Reed DB, Hardin-Fanning F. Poor sleep quality is associated with obesity and depression in farmers. Public Health Nurs. 2019 May;36(3):270–5.
6.
Ding C, Lim LL, Xu L, Kong AP. Sleep and obesity. J Obesity Metabolic Syndr. 2018 Mar;27(1):4.
7.
Gaine ME, Chatterjee S, Abel T. Sleep deprivation and the epigenome. Front Neural Circuits. 2018 Feb 27;12:14.
8.
Lucassen EA, Piaggi P, Dsurney J, et al. Sleep extension improves neu-rocognitive functions in chronically sleep-deprived obese individuals. PloS One. 2014 Jan 15;9(1):e84832.
9.
Muscogiuri G, Barrea L, Aprano S, et al. Sleep quality in obesity: does adherence to the mediterranean diet matter? Nutrients. 2020 May 10;12(5):1364.
10.
Skjåkødegård HF, Danielsen YS, Frisk B, et al. Beyond sleep duration: Sleep timing as a risk factor for childhood obesity. Pediatric Obesity. 2021 Jan;16(1):e12698.
11.
Sasaki N, Fujiwara S, Yamashita H, et al. Association between obesity and self-reported sleep duration variability, sleep timing, and age in the Japanese population. Obesity Res Clin Practice. 2018 Mar 1;12(2):187–94.
12.
Sejbuk M, Mirończuk-Chodakowska I, Witkowska AM. Sleep quality: a narrative review on nutrition, stimulants, and physical activity as important factors. Nutrients. 2022 May 2;14(9):1912.
13.
Papatriantafyllou E, Efthymiou D, Zoumbaneas E, et al. Sleep deprivation: effects on weight loss and weight loss maintenance. Nutrients. 2022 Apr 8;14(8):1549.
14.
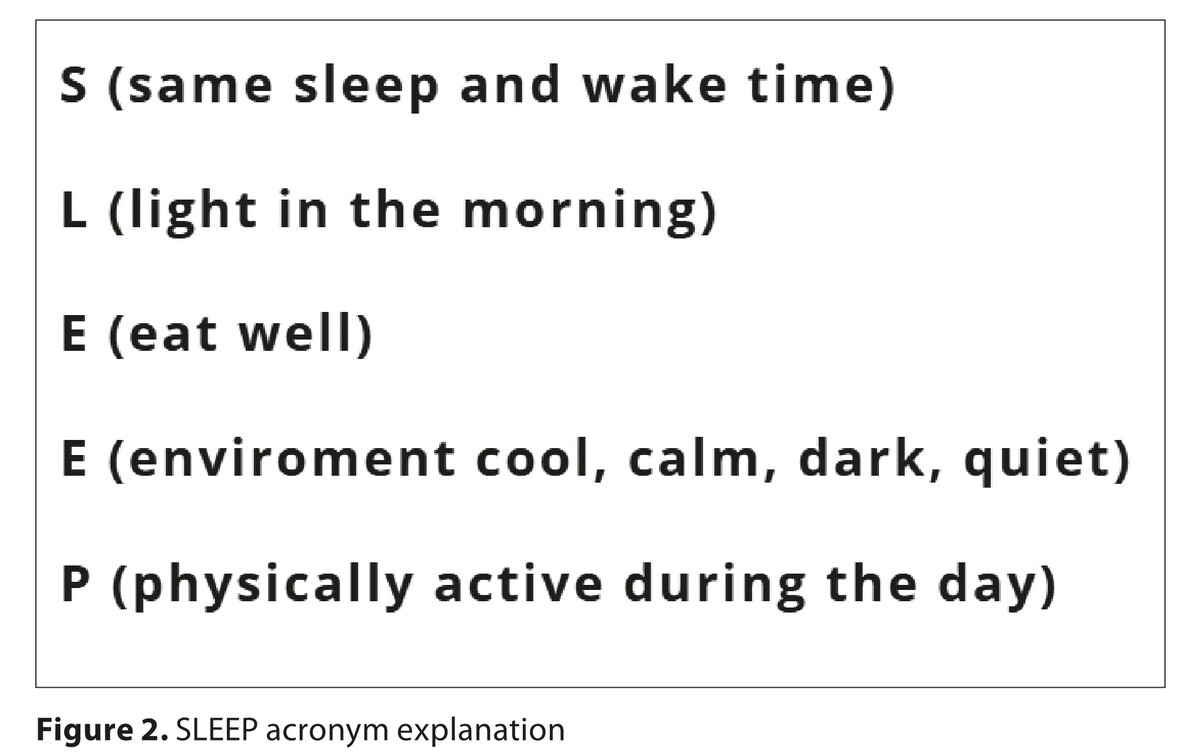
Migliaccio GM, Di Filippo G, Sancassiani F, et al. Boost Your Brainpower: 24 Daily Sleep Hacks for Active Lifestyles. Applied Sci. 2024 Jul 31;14(15):6701.
15.
Adler AB, Bliese PD, LoPresti ML, et al. Sleep leadership in the army: a group randomized trial. Sleep Health. 2021 Feb 1;7(1):24–30.
16.
Cooper CB, Neufeld EV, Dolezal BA, Martin JL. Sleep deprivation and obesity in adults: a brief narrative review. BMJ Open Sport Exer Med. 2018 Oct 1;4(1):e000392.
17.
Liu S, Wang X, Zheng Q, et al. Sleep deprivation and central appetite regulation. Nutrients. 2022 Dec 7;14(24):5196.
18.
Feingold CL, Smiley A. Healthy sleep every day keeps the doctor away. Inter J Environ Res Public Health. 2022 Aug 29;19(17):10740.
19.
Brzecka A, Sarul K, Dyła T, et al. The association of sleep disorders, obesity and sleep-related hypoxia with cancer. Curr Genomics. 2020 Sep 1;21(6):444–53.
20.
Broussard JL, Klein S. Insufficient sleep and obesity: cause or consequence. Obesity. 2022 Oct;30(10):1914–6.
21.
Piekarska M, Pszczółka M, Parol D, et al. Sleeping disorders in healthy individuals with different dietary patterns and bmi, questionnaire assessment. Inter J Environ Res Public Health. 2021 Nov 23;18(23):12285.
22.
Patel SR, Hayes AL, Blackwell T, et al. The association between sleep patterns and obesity in older adults. Inter J Obesity. 2014 Sep;38(9):1159–64.
23.
Felső R, Lohner S, Hollódy K, et al. Relationship between sleep duration and childhood obesity: systematic review including the potential underlying mechanisms. Nutrition Metab Cardiovasc Dis. 2017 Sep 1;27(9):751–61.
24.
St-Onge MP. Sleep–obesity relation: underlying mechanisms and consequences for treatment. Obesity Rev. 2017 Feb;18:34–9.
25.
Jehan S, Zizi F, Pandi-Perumal SR, et al. Obstructive sleep apnea and obesity: implications for public health. Sleep medicine and disorders: Inter J. 2017;1(4).
26.
Antza C, Kostopoulos G, Mostafa S, et al. The links between sleep duration, obesity and type 2 diabetes mellitus. J Endocrinol. 2022 Feb 1;252(2):125–41.
27.
Hjorth MF, Quist JS, Andersen R, et al. Change in sleep duration and proposed dietary risk factors for obesity in D anish school children. Pediatric Obesity. 2014 Dec;9(6):e156–9.
28.
Miller MA, Bates S, Ji C, Cappuccio FP. Systematic review and meta-analyses of the relationship between short sleep and incidence of obesity and effectiveness of sleep interventions on weight gain in preschool children. Obesity Rev. 2021 Feb;22(2):e13113.
29.
Kurnool S, McCowen KC, Bernstein NA, Malhotra A. Sleep apnea, obesity, and diabetes—an intertwined trio. Curr Diabetes Rep. 2023 Jul;23(7):165–71.
30.
Kim LJ, Alexandre C, Pho H, et al. Diet-induced obesity leads to sleep fragmentation independently of the severity of sleep-disordered breathing. J Appl Physiol. 2022 Dec 1;133(6):1284–94.
31.
Liao Z, Chen Y, Wu L, et al. Associations of obstructive sleep apnea risk with obesity, body composition and metabolic abnormalities in school-aged children and adolescents. Nutrients. 2024 Jul 25;16(15):2419.
32.
Carriere C, Coste O, Meiffred-Drouet MC, et al. Sleep disorders in obese children are not limited to obstructive sleep apnoea syndrome. Acta Paediatrica. 2018 Apr;107(4):658–65.
33.
Mogavero MP, Godos J, Grosso G, et al. Rethinking the Role of Orexin in the Regulation of REM Sleep and Appetite. Nutrients. 2023 Aug 22;15(17):3679.
34.
Miller AL, Lumeng JC, LeBourgeois MK. Sleep patterns and obesity in childhood. Curr Opinion Endocrinol Diabet Obesity. 2015 Feb 1;22(1):41–7.
35.
Gohil A, Hannon TS. Poor sleep and obesity: concurrent epidemics in adolescent youth. Frontiers Endocrinol. 2018 Jul 10;9:364.
36.
Castro AI, Gomez-Arbelaez D, Crujeiras AB, et al. Effect of a very low-calorie ketogenic diet on food and alcohol cravings, physical and sexual activity, sleep disturbances, and quality of life in obese patients. Nutrients. 2018 Sep 21;10(10):1348.
37.
Sun W, Yuan J, Yu Y, et al. Poor sleep quality associated with obesity in men. Sleep and Breathing. 2016 May;20:873–80.
38.
Song Y, Gong L, Lou X, et al. Sleep-Body Composition Relationship: Roles of Sleep Behaviors in General and Abdominal Obesity in Chinese Adolescents Aged 17–22 Years. Nutrients. 2023 Sep 25;15(19):4130.
Udostępnij
ARTYKUŁ POWIĄZANY
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.