Online first
Bieżący numer
O czasopiśmie
Archiwum
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Bazy indeksacyjne
Komitet Redakcyjny
Recenzenci
2024
2023
2022
2021
2020
2019
2018
Kontakt
Klauzula przetwarzania danych osobowych (RODO)
PRACA ORYGINALNA
Efekt krótkotrwałej ekspozycji na pył zawieszony (PM2,5 oraz PM10) oraz jego wpływ na nagłe zaostrzenia wybranych chorób układu krążenia i oddechowego we Wrocławiu w latach 2009–2013 na
podstawie rejestru wyjazdów Pogotowia Ratunkowego
1
Uniwersytet Medyczny we Wrocławiu, Polska
2
Narodowy Instytut Zdrowia Publicznego – Państwowy Zakład Higieny, Warszawa, Polska
Autor do korespondencji
Med Srod. 2019;22(3-4):49-56
SŁOWA KLUCZOWE
pył zawieszonyodpowiedź na ekspozycjewpływ krótkotrwałychoroby układu krążeniachoroby układu oddechowego
DZIEDZINY
STRESZCZENIE
W środowisku miejskim największy wpływ na zdrowie ludzi ma pył zawieszony, a będące jego efektem skutki zdrowotne zależą od jego stężenia w powietrzu, czasu narażenia oraz liczebności narażonej populacji. Wpływ ten zaznacza się zarówno jako całożyciowe narażenie na nadmierne stężenie zanieczyszczeń powietrza, jak i efekt krótkotrwałej ekspozycji prowadzącej do nagłego pogorszenia stanu zdrowia. Polskie miasta, w tym Wrocław, charakteryzują się bardzo złą jakością powietrza, co niewątpliwie ma wymierny wpływ na zdrowie
mieszkańców, zarówno w ujęciu długo, jak i krótkookresowym.
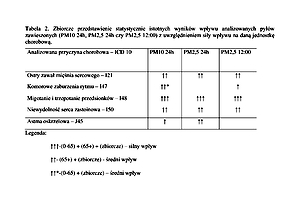
Celem pracy było określenie, jak stężenie pyłu zawieszonego w efekcie krótkotrwałej ekspozycji kształtuje ryzyko występowania stanów nagłego zagrożenia zdrowotnego (pochodzenia kardiologicznego i oddechowego). Ustalono to na podstawie rejestrów wyjazdów Pogotowia Ratunkowego we Wrocławiu w latach 2009–2013. Ryzyko analizowano w formie badania ekologicznego z użyciem analizy szeregów czasowych. Badanie wykazało, że zgłaszalność stanów nagłego zagrożenia zdrowotnego w zakresie chorób układu krążenia i układu oddechowego zwiększa się wraz ze wzrostem pyłowych zanieczyszczeń powietrza. Wzrost koncentracji pyłu zawieszonego jest szczególnie niebezpieczny dla osób powyżej 65. roku życia (65+).
In the urban environment particulate matter has the greatest impact on human health. Health effects depend on its concentration in the air, duration of exposure, and the size of the population exposed. This effect is exerted through both lifetime exposure to excessive concentrations of air pollutants, and as short-term exposure leading to sudden deterioration of the state of health. Polish cities, including Wrocław, are characterized by very poor air quality, which undoubtedly has a measurable impact on the health of inhabitants in the
long and short terms.
The aim of the study was to determine how short-term exposure to the concentration of suspended particulate matter shapes the risk of occurrence of emergency health conditions of cardiovascular and respiratory origin, based on registers of ambulance emergency calls in Wrocław, during 2009–2013. The risk was analyzed in the form of ecological study using time series analysis.
The study showed that calls for the ambulance emergency service due to cardiovascular and respiratory risk increased together with a rise in air pollution with particulate matter. An increase in the concentration of particulate matter creates special risk for people aged over 65 (65+).
REFERENCJE (41)
1.
Krzeszowiak J, Pawlas K. Zanieczyszczenie powietrza we Wrocławiu i potencjalne zagrożenie dla zdrowia z tym związane. Med Srod. 2015; 18(2): 66–73.
2.
Krzeszowiak J, Pawlas K. Pył zawieszony (PM2,5 oraz PM10), właściwości oraz znaczenie epidemiologiczne ekspozycji krótko- i długookresowej dla chorób układu oddechowego oraz krążenia. Med Srod. 2018; 21(2): 7–13.
3.
Samoli E, Peng R, Ramsay T, et al. Acute Effects of Ambient Particulate Matter on Mortality in Europe and North America: Results from the APHENA Study. Environ Health Perspect. 2008; 116: 1480–1486.
4.
Atkinson RW, Anderson HR, Sunyer J, et al. Acute Effects of Particulate Air Pollution on Respiratory Admissions Results from APHEA 2 Project. Am J Resp Critical Care Med. 2001; 164(10): 1860–1866.
5.
Le Tertre A, Medina S, Samoli E, et al. Short-term effects of particulate air pollution on cardiovascular diseases in eight European cities. J Epidemiol Comm Health. 2002; 56 721–721.
6.
Wood SN. Generalized Additive Models: An Introduction with R. Chapman and Hall/CRC Press 2006.
8.
R Core Team (2014). A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria: http://www.R-project.org/.
9.
Atkinson RW, Anderson HR, Sunyer J, et al. Acute Effects of Particulate Air Pollution on Respiratory Admissions Results from APHEA 2 Project. Am J Resp Critical Care Med. 2001; 164(10): 1860–186.
10.
Villeneuve PJ, Chen Li, Rowe BH, et al. Outdoor air pollution and emergency department visits for asthma among children and adults: A case-crossover study in northern Alberta, Canada. Environ Health. 2007; 6: 40.
11.
Riediker M, Cascio WE, Griggs TR, et al. Particulate Matter Exposure in Cars Is Associated with Cardiovascular Effects in Healthy Young Men. Am J Resp Critical Care Med. 2004; 169(8): 934–940.
12.
Link SM, Luttmann-Gibson H, Schwartz J, et al. Acute Exposure to Air Pollution Triggers Atrial Fibrillation. J Am Coll Cardiol. 2013; 62(9): 816–825.
13.
Rich DQ, Schwartz J, Mittleman MA, et al. Association of short-term ambient air pollution concentrations and ventricular arrhythmias. Am J Epidemiol. 2005; 161(12): 1123–32.
14.
He F, Shaffer ML, Rodriguez-Colon S, et al. Acute effects of fine particulate air pollution on cardiac arrhythmia: the APACR study. Environ Health Perspect. 2011; 119(7): 927–32.
15.
Dockery DW, Luttmann-Gibson H, Rich DQ, et al. Association of air pollution with increased incidence of ventricular tachyarrhythmias recorded by implanted cardioverter defibrillators. Environ Health Perspect. 2005: 670–674.
16.
Peters A, Liu E, Verrier RL, et al. Air pollution and incidence of cardiac arrhythmia. Epidemiology. 2000; 11(1): 11–17.
17.
Bunch TJ, Horne BD, Asirvatham SJ, et al. Atrial fibrillation hospitalization is not increased with short-term elevations in exposure to fine particulate air pollution. Pacing Clin Electrophysiol. 2011; 34(11): 1475–9.
18.
Milojevic A, Wilkinson P, Armstrong B, et al. Short-term effects of air pollution on a range of cardiovascular events in England and Wales: case-crossover analysis of the MINAP database, hospital admissions and mortality. Heart. 2014; 100(14): 1093–8.
19.
Wichmann HE, Mueller W, Allhoff P, et al. effects during a smog episode in West Germany in 1985. Environ Health Perspect. 1989; 79: 89.
20.
Monrad M, Sajadieh A, Christensen JS, et al. Long-Term Exposure to Traffic-Related Air Pollution and Risk of Incident Atrial Fibrillation: A Cohort Study. Environ Health Perspect. 2017; 125(3): 422–427.
21.
Atkinson RW, Carey IM, Kent A, et al. Long-Term Exposure to Outdoor Air Pollution and Incidence of Cardiovascular Diseases. Epidemiology. 2013; 24 (1): 44–53.
22.
Mordukhovich I, Kloog I, Coull B, et al. Association Between Particulate Air Pollution and QT Interval Duration in an Elderly Cohort. Epidemiology. 2016; 27(2): 284–90.
23.
Wold LE, Ying Z, Hutchinson KR, et al. Cardiovascular Remodeling in Response to Long-Term Exposure to Fine Particulate Matter Air Pollution. Circulation: Heart Failure. 2012.
24.
Sun Q, Wang A, Jin X. Long-term air pollution exposure and acceleration of atherosclerosis and vascular inflammation in an animal model. JAMA J Am Med Assoc. 2005; 294: 3003–3010.
25.
Campen MJ, Babu NS, Helms A. Nonparticulate components of diesel exhaust promote constriction in coronary arteries from ApoE−/− mice. Toxicol Sci. 2005; 88: 95–102.
26.
Zeka A, Sullivan JR, Vokonas PS, et al. Inflammatory markers and particulate air pollution: characterizing the pathway to disease. Int J Epidemiol. 2006; 35: 1347–1354.
27.
Chuang KJ, Chan CC, Su TC, et al. The effect of urban air pollution on inflammation, oxidative stress, coagulation, and autonomic dysfunction in young adults. Am J Respir Crit Care Med. 2007; 176: 370–37.
28.
Mustafic H, Jabre P, Caussin C, et al. Main air pollutants and myocardial infarction: a systematic review and meta-analysis. JAMA. 2012; 307(7): 713–721.
29.
Tonne C, Melly S, Mittleman M. et al. A case-control analysis of exposure to traffic and acute myocardial infarction. Environ Health Perspect. 2007; 115(1): 53–57.
30.
Peters A, von Klot S, Heier M, et al. Exposure to traffic and the onset of myocardial infarction. New England J Med. 2004; 351(17): 1721–1730.
31.
Nawrot TS, Perez L, Künzli N, et al. Public health importance of triggers of myocardial infarction: a comparative risk assessment. The Lancet. 2011; 377(9767): 732–740.
32.
Stafoggia M, Cesaroni G, Peters A, et al. Long-Term Exposure to Ambient Air Pollution and Incidence of Cerebrovascular Events: Results from 11 European Cohorts within the ESCAPE Project. Environ Health Perspect. 2014; 122(9): 919–925.
33.
Luo C, Zhu X, Yao C, Hou L, Zhang J, et al. Short-term exposure to particulate air pollution and risk of myocardial infarction: a systematic review and meta-analysis. Environ Sci Pollut Res Int. 2015; 22(19): 14651–62.
34.
Bhaskaran K, Hajat S, Armstrong B, et al. The effects of hourly differences in air pollution on the risk of myocardial infarction: case crossover analysis of the MINAP database. BMJ. 2011; 343.
35.
Newby DE, Mannucci PM, Tell GS, et al. Expert position paper on air pollution and cardiovasculardisease. European Heart J. 2014; 36(2): 83–93.
36.
Pope CA, Renlund DG, Kfoury AG, et al. Relation of heart failure hospitalization to exposure to fine particulate air pollution. Am J Cardiol. 2008; 102(9): 1230–4.
37.
Wellenius GA, Bateson TF, Mittleman MA, et al. Particulate Air Pollution and the Rate of Hospitalization for Congestive Heart Failure among Medicare Beneficiaries in Pittsburgh, Pennsylvania. Am J Epidemiol. 2005; 161(11): 1030–1036.
38.
Yang C, Chen A, Chen R, et al. Acute effect of ambient air pollution on heart failure in Guangzhou, China. Int J Cardiol. 2014; 177(2): 436–41.
39.
Forastiere F, Agabiti N. Assessing the link between airpollution and heart failure. The Lancet 2013; 382(9897): 1008–1010.
40.
Shah AS, Langrish JP, Nair H, et al. Global association of air pollution and heart failure: a systematic review and meta-analysis. Lancet. 2013; 382(9897): 1039–48.
41.
Wellenius GA, Schwartz J, Mittleman MA. Particulate air pollution and hospital admissions for congestive heart failure in seven United States cities. Am J Cardiol. 2006; 97(3): 404–8.
Udostępnij
ARTYKUŁ POWIĄZANY
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.